With evolving stent technology, improvements in percutaneous coronary intervention (PCI) techniques and the use of antithrombotic medications, the role of PCI in the treatment of left main stem (LMS) disease has expanded from being confined to salvage scenarios to intermediate- and lower-risk patients. However, the role and benefits of coronary artery bypass grafting (CABG) surgery in the treatment of multivessel disease and LMS disease have been well established with long-term follow-up. In order to assess the role and efficacy of PCI in LMS disease compared with CABG, several randomised clinical trials have been performed. In this review, some of the earlier and later trials will be compared. In recent months, one of them – the Evaluation of XIENCE Versus Coronary Artery Bypass Graft Surgery for Effectiveness of Left Main Revascularization (EXCEL) trial – has attracted a significant amount of scientific and media attention.1 This review will outline the methodology of EXCEL, as well as other trials on the management of LMS disease and summarise the debates around EXCEL including statements from professional societies as well as the impact of these trials on real-world practice.
PCI Versus CABG for the Treatment of Left Main Stem Disease
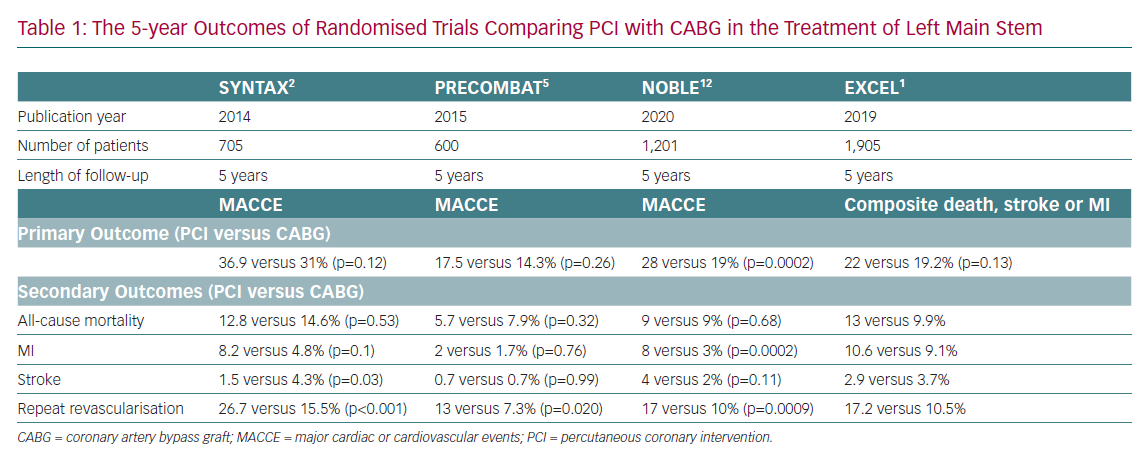
Earlier trials demonstrated the efficacy and safety of first-generation drug-eluting stents (DES) and later trials compared the second-generation DES with CABG. The outcome measures used in these trials include the occurrence of major adverse cardiac and cerebrovascular events (MACCE) at short and medium term, early and late mortality of cardiac and all-cause reasons, complete revascularisation at the time of primary procedure and rate of repeat revascularisation during follow-up. The trials include Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX), Premier of Randomized Comparison of Bypass Surgery Versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease (PRECOMBAT), Left Main Coronary Artery Stenting (LEMANS), Nordic Baltic British Left Main Revascularisation (NOBLE) and EXCEL.2–6
Evidence from the SYNTAX trial showed the benefits of CABG in LMS with a SYNTAX score of >32.2,3 However, in patients with a SYNTAX score of <32, PCI and CABG showed similar results. The SYNTAX trial was not powered to address the efficacy of PCI versus CABG and therefore further studies like NOBLE and EXCEL were needed. EXCEL and NOBLE are non-inferiority randomised trials designed to compare and evaluate the efficacy of PCI and CABG in patients with LMS disease.
The SYNTAX Trial
The SYNTAX trial was a multicentre randomised controlled trial of 1,800 patients with three-vessel or LMS disease comparing CABG with PCI using Taxus Express paclitaxel-eluting stents (Boston Scientific).2 A non-inferiority comparison of the primary endpoint of MACCE was undertaken at 1 and 5 years. The 5-year results were published in 2014.7
In the LMS subgroup (n=705) there were no significant differences in mortality at 5 years (12.8% PCI versus 14.6% CABG; p=0.53), the occurrence of MACCE (36.9% PCI versus 31% CABG; p=0.12) and MI (8% PCI versus 5% CABG). However, CABG had a higher stroke rate (1.5% PCI versus 4.3% CABG; p=0.05) and PCI had a significantly higher rate of repeat revascularisation (26.7% PCI versus 15.5% CABG; p<0.001). In patients with high SYNTAX scores, MACCE was significantly increased with PCI (high score, 46.5% PCI versus 29.7% CABG; p=0.003).8 At 10 years, no significant difference existed in all-cause death between PCI and CABG. However, CABG provided a significant survival benefit in patients with three-vessel disease, but not in patients with LMS disease.9
The SYNTAX Score and its Role
The SYNTAX score is a method of quantifying the angiographic appearance of coronary artery lesions based on their anatomical location and complexity to treat by PCI. It is an additive score of all the lesions and therefore reflects the quantity of myocardium at risk. It has been shown to be predictive of adverse outcomes following PCI but less so after CABG, since the success of CABG does not only depend on the lesions themselves, but also on nature of the coronary lesions among other factors.10
It must be remembered that as a static, non-physiological anatomical score it does not take account of patient factors, such as comorbidities, cardiac function or patient preference. Although current European guidelines recommend the SYNTAX score as an assessment of severity of coronary artery disease, they do not recommend its routine use to determine PCI versus CABG.11 SYNTAX scoring should be interpreted with caution in the context of a balanced multidisciplinary team (MDT).
PRECOMBAT
The PRECOMBAT trial was a randomised controlled trial of 600 patients with unprotected LMS disease to undergo PCI with a sirolimus-eluting stent or CABG. Once again this was a non-inferiority study, with the primary endpoint being MACCE.4,5 In PRECOMBAT, mortality at 5 years was 5.7% for PCI versus 7.9% for CABG (p=0.32) and MACCE was 17.5% for PCI versus 14.3% for CABG (p=0.26). The incidence of MI (2% PCI versus 1.7% CABG; p=0.76) and stroke (0.7% PCI versus 0.7% CABG; p=0.99) were not significantly different. However, as in the SYNTAX trial, the rate of repeat revascularisation was higher in the PCI group (13.0% PCI versus 7.3% CABG; p=0.020).
NOBLE
NOBLE was a prospective, randomised, open-label, non-inferiority trial carried out at 36 hospitals in nine northern European countries.12,13 A total of 1,201 patients with LMS disease requiring revascularisation were enrolled and randomly assigned (1:1) to receive PCI or CABG.
Of note, NOBLE did not use SYNTAX score as a criterion, but instead excluded patients with more than three additional coronary lesions or more complex coronary lesions. A total of 598 patients were allocated to PCI and 603 to CABG. At 5 years, all-cause mortality and cardiac death occurred in 9% and were the same after both procedures with MACCE rates of 28% for PCI versus 19% for CABG (p=0.0002). The latter exceeded the non-inferiority threshold and CABG was significantly better than PCI. Non-procedural MI was higher after PCI (8% PCI versus 3% CABG; p=0.0002). Patients treated with PCI had higher rates of repeat revascularisation (17% PCI versus 10% CABG; p=0.0009).12
EXCEL
The EXCEL trial is a prospective, randomised, open-label, non-inferiority trial of 1,905 patients of low or intermediate anatomical complexity. A total of 948 patients received fluoropolymer-based-cobalt-chromium everolimus-eluting stent and 957 underwent CABG. At 3 years, death, stroke, MI or revascularisation occurred in 23.1% of the patients in the PCI group and in 19.1% in the CABG group (p=0.01 for noninferiority; p=0.10 for superiority).14
In the EXCEL trial at 5 years, the authors reported that a primary outcome event had occurred in more patients with PCI, but this was not significant (22.0% PCI versus 19.2% CABG; p=0.13).1 However, the incidence of all-cause mortality was significantly higher in the PCI group (13.0% PCI versus 9.9% CABG, OR 1.38, 95% CI [1.03–1.85]). The incidences of cardiovascular death (5.0% PCI versus 4.5% CABG, 0.5 percentage points, OR 1.13) and MI (10.6% PCI versus 9.1% CABG) were not significantly different. All cerebrovascular events were less frequent after PCI than after CABG (3.3% PCI versus 5.2% CABG; −1.9 percentage points; OR 0.61), although the incidence of stroke was not significantly different (2.9% versus 3.7%; −0.8 percentage points; OR 0.78). They report that repeat revascularisation was more frequent after PCI than after CABG (17.2% versus 10.5%). The authors conclude that there was no significant difference between PCI and CABG in respect of the composite outcome of death, stroke or MI at 5 years.
EXCEL and NOBLE have shown contradictory results both at 3- and 5-year follow-up. This is probably related to their inclusion criteria, possible crossover of patients in EXCEL from PCI group to CABG between 3 and 5 years and several other factors, which are argued comprehensively by Park et al.15 A summary of these trials is shown in Table 1.
Non-inferiority Trials
Randomised controlled trials are thought to be the gold standard in comparing two modalities of treatment compared to registries, which may or may not be propensity matched. The main strength of a randomised controlled trial is avoiding bias. However, there are several weaknesses, including a very small number of potentially eligible patients who can be included resulting in only a small number of patients being studied, atypical patient populations, short duration of follow-up, large number of crossovers and being expensive. In contrast, registries can recruit large number of patients, represent real-world practice and they are relatively cheap. However, they suffer from bias and confounding factors at various levels.
There has been an explosion of non-inferiority trials in cardiovascular diseases like the trials described in this paper. Bikdeli et al. report that non-inferiority cardiovascular trials are increasingly being published by the highest impact journals, with 79% funded by private industries and 8% funded by non-profit organisations.16 Between 1990 and 2016, 111 cardiovascular non-inferiority trials were published. Eighty-six of these trials, many of which were large multicentre studies, claimed tested new interventions were non-inferior to the compared therapy and only eight demonstrated inferiority.
Adverse Media Attention
The publication of the EXCEL trial was followed by serious concerns raised about its methodology and the integrity of its results.17–19 The trial was the subject of a BBC Newsnight programme in December 2019.20 The programme raised concerns about the validity of the conclusions of the trial, whether important data had been withheld, and raised the possibility that the study was inherently flawed from the outset because of conflicts of interest amongst the investigators, given that it had been financed by stent manufacturers.
As a result of these very serious allegations, the European Association of Cardiothoracic Surgery (EACTS) and European Society of Cardiology (ESC) guideline group withdrew their support for the joint EACTS/ESC statement on the management of patients with LMS disease, until a full independent analysis of the EXCEL trial data had been carried out.18,19 EACTS summarised its concerns because of the 35% increased risk of death in the PCI group, failure of the authors to publish the data using the Universal Definition of MI, emerging mortality data that was available to the data safety monitoring board not being made available to the guideline task force and alleged conflict of interest. Later, in a letter to EXCEL primary investigators, Domenico Pagano on behalf of EACTS invited the authors to make the raw data available to the Clinical Trials Unit at University College London for re-analysis.19
The British Cardiovascular Intervention Society (BCIS) also released a statement on 11 December 2019 reassuring the patients undergoing stent procedures and that patients with LMS disease will be discussed by a multidisciplinary heart team and the outcome of this discussion will be shared with patients in order to reach a final decision.21
The president of the Society for Cardiothoracic Surgery (SCTS), Mr Richard Page, wrote on 18 December 2019: “A number of colleagues are understandably concerned that the joint statement [by SCTS, British Cardiovascular Intervention Society and British Cardiovascular Society] did not clarify the current situation/evidence for the treatment of Left Main Stem stenosis, given that doubts have been raised about the integrity of Excel.22,23 There was uncertainty within the cardiac surgical community as to the position taken by the SCTS. Clearly an explanation is required, which is why I am writing to you again. Very soon after the Newsnight programme we were made aware of patients and relatives who were concerned as to whether they were receiving the right treatment, even to the extent that some were questioning if stents were safe in any situation. Therefore there was a real and pressing need to be able to reassure patients and their families that they could trust cardiovascular physicians and surgeons in the UK to give balanced and appropriate advice, and that each and every patient will have access to specific and individualised treatment, notwithstanding the questions raised regarding the validity of the Excel trial. We did not feel that a statement from SCTS alone would be constructive to the situation and it would be more sensible and reassuring to patients, relatives and the NHS to see collaboration and a joint statement from the professional societies that are responsible for all aspects of decision making in this pattern of coronary disease.”
A further letter to SCTS members from the President on 17 February 2020 provided an update on the situation: “The SCTS agrees with EACTS (and indeed all other cardiothoracic surgical societies throughout the world who have expressed an opinion) that on current evidence coronary bypass surgery is superior to stenting in the treatment of the vast majority of patients with LMSS and remains the best treatment that we can offer. Nevertheless when the risks of surgery are significant, stenting for LMSS may be a safer alternative in some circumstances.”
Many of our patients understandably find the adverse media attention and various statements confusing and worrying. We discuss this in more detail in the Patient’s Choice section. Unpublished data of a survey of the understanding of patients of the extent and nature of their coronary artery disease shows that almost no patient can tell the difference between LMS disease, triple vessel disease and/or significant coronary artery disease.
Controversies of the EXCEL Trial
There are several controversies of the methodology and conduct of the EXCEL trial that have been addressed, including the following:16,24
- The EXCEL investigators use the Society for Cardiovascular Angiography and Interventions (SCAI) definition of peri-procedural MI rather than the Universal Definition of MI.25,26 The use of SCAI caused the reporting of 37% higher occurrence of MI in the CABG group. Furthermore, the use of Universal Definition of MI would have allowed a fairer comparison of EXCEL with other trials. In addition, Ruel et al. showed that the SCAI definition of MI exaggerated procedural MI after CABG.27
- The incidence of all-cause mortality was significantly higher in the PCI group (13.0% PCI versus 9.9% CABG; OR 1.38; 95% CI [1.03–1.85]). There is an increasing divergence during the follow-up period for death in favour of CABG. At 5 years, the mortality rate was significantly higher in the PCI group compared to CABG. The EXCEL investigators had classified all-cause mortality as a secondary endpoint and reported that its statistical significance was uncertain. The majority of the trials have all-cause mortality as a primary endpoint and therefore hiding of all-cause mortality is disingenuous.
- Repeat revascularisation, which has been shown to be an independent predictor of death, MI and stroke, was significantly higher in the PCI group.28 Repeat revascularisation as an outcome measure has significant implications for patient’s quality of life and health service economy and has been used as a primary outcome measure in earlier trials.29,5 We believe that repeat revascularisation should have been considered as primary endpoint. Furthermore, repeat revascularisation during follow-up was performed less frequently after CABG than PCI and was associated with increased mortality after both procedures.30
- The HR of the composite of death, stroke and MI shifted from being in favour of PCI at 30 days to CABG during the follow-up period. This indicates that CABG is the preferred option in patients with longer life expectancy.
- Unlike the PCI group, the CABG group was heterogeneous in both using off-pump technique and arterial grafting. Overall 29.4% of the CABG operations were off-pump. In a subgroup analysis, Benedetto et al. reported a significantly higher all-cause mortality in the off-pump compared to on-pump patients at 3 years (8.8% off-pump versus 4.5% on-pump).31
Furthermore, there is strong evidence in patients undergoing CABG for the use of multiple arterial grafting improving survival.32–35 However, only 24% of patients in EXCEL received bilateral mammary arteries and 6% received radial arteries. In such a heterogeneous population, it is difficult to assess the impact of the known benefits of arterial revascularisation.36 These factors should be taken into account when analysing the EXCEL data.
Assessment of Left Main Stem
Coronary angiography has traditionally been the gold-standard for diagnosis of coronary artery disease and uses anatomical evaluation of the coronary arteries through multiple angiographic views and thereby identify stenoses that necessitate further intervention.37 Studies have demonstrated a poor correlation between angiographic appearance of a coronary artery to the true degree of stenosis in some cases which can be observer dependent.38
Fractional flow reserve (FFR) has been increasingly used along with angiography in PCI. FFR is measured during coronary catheterisation by passing a pressure-monitoring guide wire distal to the coronary lesion and inducing maximal hyperaemia, usually through intravenous or intracoronary adenosine administration to cause vasodilation.39 It measures the drop in perfusion pressure across a stenosis, therefore representing its physiological effect on myocardial blood flow. Its use is widespread in PCI, though its role in CABG remains uncertain. We carried out a systematic review and meta-analysis to evaluate current evidence on outcomes following FFR-guided CABG compared to angiography-guided CABG.40 We showed that there was no reduction in repeat revascularisation or postoperative MI with FFR. In addition, FFR-guided CABG provided a reduction in mortality, but this was not reported to be due to cardiac causes. There may be a role for FFR in CABG, but large-scale randomised trials are required to establish its value.
The Role of the Multidisciplinary Team Meeting
“The mind is an attribute of the individual. There is no such thing as a collective brain. The primary act – the process of reason – must be performed by each man alone. We can divide a meal among many men. We cannot digest it in a collective stomach. No man can use his lungs to breathe for another man. No man can use his brain to think for another.”
The Fountainhead, Ayn Rand, 1943
The Heart Team is an integral part of the patient care pathway for those with complex coronary artery disease. In 2014, the first joint ESC/EACTS guidelines on myocardial revascularisation were published to help inform Heart Teams of current best evidence on the topic.41 In 2013, Head et al. reported that the concept of the Heart Team was not widely implemented. Decision-making was shown to remain suboptimal, there was large variability in PCI to CABG ratios, which could have been predominantly the consequence of physician-related factors, raising concerns regarding overuse, underuse and inappropriate selection of revascularisation.42
Our group showed that despite the introduction of joint cardiology and surgical international guidelines, a significant number of patients were receiving inappropriate PCI against those guidelines.43
Subsequent guidelines in 2018 specifically recommend the use of Heart Team for decision making in patients with coronary artery disease.10 They give a Class 1C recommendation (meaning it is recommended or indicated based on expert opinion) for interdisciplinary protocols for common case scenarios to implement the appropriate revascularisation strategy in accordance with current guidelines. Furthermore, they state individual discussion should occur for all complex cases and that the Heart Team should provide a balanced multidisciplinary decision-making process.
This decision-making process is guided by the combined personal experience of the Heart Team in conjunction with current best evidence. Evidence obtained from large randomised controlled trials will often be relied upon by the Heart Team. Therefore, it is imperative that such studies have been conducted with integrity and the results reported accurately.
Assessing the effectiveness and reproducibility of a coronary Heart Teams decisions is difficult. A study from the UK has previously shown that 93% of decisions on 399 patients are implemented and when re-discussed at a later date 80% of decisions are unchanged.44 This of course does not account for patients who are treated without the benefit of Heart Team discussion.
In day-to-day practice, clinicians are unable to discuss the nuanced findings of these trials for each patient. Therefore, the role of Heart Team and MDT have been emphasised.45,42
In the UK, CABG comprises approximately 40% of the adult cardiac surgery operations per annum. A total of 14,527 isolated non-emergency CABG operations were performed between April 2017 and March 2018.46 However, data are not available as to what proportion had LMS disease. Similarly, there is a significant number of PCIs performed for multivessel disease, but it is difficult to extract from the BCIS database what percentage had LMS disease. The question is whether every single patient with LMS can be discussed in an MDT with Heart Team setting.
The authors of this article suspect that only a small proportion of LMS patients are discussed at MDTs. The treatment decision is clinician-dependent and is often related to the culture of a unit. Unfortunately, the decision around management of LMS patients can often become dominated by a discussion around technical feasibility of PCI. This conflation of two separate issues may not always be in the wider interest for patients with this disease.
The Patient’s Choice
It is difficult for clinicians – let alone patients – to navigate their way around these complex trials with their inherently nuanced conclusions. Patients need accurate information in order to make an informed decision. The quality of any discussion can influence which decision is reached. Many patients exhibit a high degree of suggestibility, meaning that it is possible to influence their decision-making in a particular direction, depending on how or even the order in which information is relayed. An example of this is if a patient is asked if they would like a procedure that will help them. The proposed procedure is not surgery, but similar to an angiogram, and they could go home soon after. This is then contrasted with major cardiac surgery, describing a midline chest incision, deliberately stopping the heart, multiple limb incisions and a 1-week hospital stay plus a total recovery time of 3 months.
What may be perceived by cardiologists as a prohibitive risk for surgery, then becomes conflated with patient choice. Four pillars of medical ethics ensure that, when considered together, everyone receives the same standard of healthcare. The same principles also serve to provide guidance to doctors in approaching the care of their patients. These four pillars are autonomy, beneficence, non-maleficence and justice. The founding ethical principle that is mainly undermined in the above scenarios is patient autonomy. That is, the universal right of competent adults to make informed decisions about their own medical care. Thus, by failing to appraise patients properly of the risks and benefits of all treatments, including no treatment, patient choice is suddenly transformed, to something more akin to dealer’s choice. For the uninitiated, the latter phrase also describes a particular style of poker, where each player may deal a different variant.
Informed Decision-making
In view of some of the controversies highlighted by the EXCEL trial data and its natural extrapolation to the management of coronary artery disease in general, there is perhaps now an opportunity to improve the role of the MDT/Heart Team. A more systematic approach would be to openly discuss all patients with LMS who require elective coronary intervention, with a structured proforma completed in each case. Essential information should include presence of important risk factors such as diabetes, defining the vessels to be grafted, potential benefits of complete versus incomplete revascularisation, therefore possibility and extent of arterial grafting and consultation by both the cardiologist and the cardiac surgeon. The Heart Team meeting should have an agreed attendance of cardiologists, surgeons and others to achieve quoracy. It would also benefit from a neutral chair. The final decision as to the mode of treatment should be based on real-world evidence and not “let’s wait for the next generation of stents and use of multiple and stronger anti-platelet medications”. Facts emerging from the most recent trials have not, by and large, been catalysed by newer stent technology.
Conclusion
We have attempted to set out the context of the recent events that have led to confusion. The SYNTAX trial was the first randomised trial to compare CABG and PCI in patients with complex coronary disease. The definitive results confirmed that CABG should remain the standard of care for patients with complex coronary lesions. For patients with less complex lesions, or LMS disease, SYNTAX found that PCI is an acceptable alternative, even though it was not designed to assess the overall efficacy of PCI versus CABG. It was against this background, that the EXCEL trial was designed to investigate the newer-generation DES versus CABG in patients with low-risk or intermediate-risk LMS disease. The initial conclusion of the EXCEL authors, that there was no significant difference between PCI and CABG in respect of the composite endpoints of death, stroke or MI at 5 years, has subsequently been called into question. This is related to controversies regarding the trial methodology, disagreements about which definition of peri-procedural MI was used and alleged investigator conflicts of interest. The EXCEL debacle has, to some extent, undermined public confidence in medical research in general and in clinical trials in particular.
It is unlikely that there will be a further large randomised trial aimed at addressing the issue of the optimum method of revascularisation for LMS disease but further subgroup analyses from these trials may be hypothesis generating.
There are already good quality data that suggest CABG confers a survival advantage for patients with LMS disease. Most authors recommend genuine discussions take place between cardiologists and cardiac surgeons regarding optimal treatment for complex coronary artery disease or LMS disease. This does not always happen in the way that it should. In some cases the invasiveness of CABG is emphasised to engineer patient choice in favour of PCI.
We advocate a systematic approach to the Heart Team Meeting, with a structured proforma, agreed quorum and a neutral chair. We must apply judicious management to coronary artery disease. Who should lead this clarion call? We invite key opinion leaders of cardiac surgery and cardiology, namely their respective professional organisations, to rise to the challenge of ensuring the treatment of particularly LMS patients is based on sound ethical and scientific principles. We owe this much to our patients; nothing less will suffice and they are the ultimate beneficiaries.