Despite recent advancements in the area of cardiovascular disease, the burden of disease accompanying acute coronary syndrome (ACS) remains extensive. Expeditious identification and intervention are central to positive patient outcomes, and symptom recognition is fundamental for both patients in initiating health-seeking behaviour and clinicians in governing their clinical approach.1,2 A firm understanding of the various symptomologies and their risk factors is instrumental in generating suspicion for ACS early in the clinician-patient exchange; this facilitates appropriate actions including apposite triage, direct, fastidious historytaking with germane physical evaluation and prompt initiation of further clinical exploration.3 Such processes inform timely, accurate diagnosis, culminating in the direction of subsequent treatment trajectories and improved patient outcomes.4
Retrosternal chest pain or discomfort is the most widely documented and identifiable leading symptom of ACS so is useful when initiating diagnostic and therapeutic activity.5 However, despite chest pain being a cardinal symptom, it has been shown to have limited diagnostic and prognostic value, with some arguing other symptoms suggestive of myocardial ischaemia – anginal equivalents – possess a higher diagnostic value for acute MI.6,7
Sentinel studies suggest presentations without cardiac chest pain are not uncommon, with one large multicentre study reporting 33% of acute MI patients presented without cardiac chest pain and another investigating unstable angina (UA) identifying this in more than half of patients (52%).8,9 Current evidence suggests poor outcomes for patients presenting without cardiac chest pain, including longer prehospital delay, delayed diagnosis, lower likelihood of receiving a confirmed diagnosis of MI at admission, greater hospital complications, less guideline-driven medication and reperfusion efforts, and higher mortality rates.10-12
Older age, female sex, ethnicity, comorbidities such as diabetes and hypertension, previous medical events, including stroke and acute MI, are often believed to be associated with such presentations.8 However, these findings are not uniform across studies, so clarity surrounding predisposing risk factors associated with ACS presentations without cardiac chest pain has proven elusive.13 Consequently, these patients remain a largely underresearched and poorly understood cohort with an enduring enigmatic status.
A lack of clear definitions and systematic data collection methods are the likely explanation for this, hence the need for comprehensive review and update. Various descriptors such as typical chest pain, atypical chest pain and atypical symptoms have been used throughout the literature and clinical practice in past two decades. However, use of the term atypical has recently been discouraged in clinical guidelines, with experts arguing this is misleading and inaccurate as it may refer to symptoms considered non-ischaemic or non-cardiac.14,15
As new research that adopts the lexicon featured in the guidelines emerges, it is anticipated this will be reflected in future literature accordingly. However, to avoid confusion in this review, we retain the use of atypical chest pain aligned with its use in the literature reported herein and define atypical chest pain as that incorporating descriptors including sharp, stabbing, pleuritic, burning or positional. Similarly, atypical symptoms include anginal equivalents or symptoms that are not related to thoracic pain or discomfort.
Equitable and best patient care starts with greater awareness of presentations beyond ischaemic cardiac chest pain. However, what those symptoms are, their proportions and risk factors have yet to be systematically collated and reported. Subsequently, a better understanding of the varying symptomology of ACS has the potential to advise public health campaigns, inform clinical guidelines, encourage early health-seeking behaviour and support clinicians in their approach and decision-making.16 As such, research to identify what the constellation of symptoms suggestive of myocardial ischaemia are is vital. Hence, the aims of this scoping review were to systematically investigate and collate: definitions of presentations other than cardiac chest pain in ACS patients; atypical chest pain and anginal equivalent symptoms reported and their proportions; risk factors in presentations without cardiac chest pain; and lastly, outcomes for ACS patients presenting without cardiac chest pain and comparing those with patients experiencing cardiac chest pain.
Methods
As the aims for this review were broad, a scoping review approach was adopted.17 This scoping review was conducted in line with the Joanna Briggs Institute guide to conducting scoping reviews, and written in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR).18,19
Our operational definitions for this review included: atypical chest pain, incorporating descriptors of non-specific, sharp, stabbing, pleuritic, burning or positional. Therefore, this excludes presentations of cardiac chest pain defined as ‘classic chest discomfort that is based on quality, location, radiation, provoking and relieving factors’ and is used where the term typical chest pain would have been used previously.14 Descriptors often used for typical chest pain include pressure, tightness, squeezing, heaviness or aching.14 Atypical symptoms are referred to as anginal equivalents and incorporate pain at a location other than the chest, or other symptoms, such as dyspnoea, diaphoresis, nausea and syncope. Within the recent literature, before the publication of recent definitional guidelines, these symptoms are often referred to as atypical, non-classical or non-chest pain. Therefore, the terms typical and atypical appear in the current review.14,15
Inclusion Criteria
To meet inclusion criteria, articles were required to report and explicate any symptomology among adult patients with a confirmed diagnosis of ACS presenting without cardiac chest pain (i.e. atypical chest pain or atypical symptoms/anginal equivalents).16 Articles had to be available in English language and full text and published in peer-reviewed journals, and no limiters regarding methodology were used. Limiters of adults (aged >18 years) and publication from the year 2000 were applied; the date limit was selected to coincide with marked changes within the study of ACS.20,21 ACS was defined as a confirmed clinical diagnosis of acute MI, ST-elevation MI (STEMI), non-ST-elevation MI (NSTEMI) or UA.22
Exclusion Criteria
Articles were excluded if they failed to clearly report symptoms independent of cardiac chest pain, specifically silent ACS presentations or where symptoms were reported in aggregate with chest pain and did not allow for extrapolation of data separately from chest pain reports (i.e. accompanying symptoms). Conference abstracts, case studies and reviews were also excluded; however, a hand search of excluded review references was undertaken.
Information Sources
The electronic databases MEDLINE, CINAHL, Scopus and Embase were systematically searched by one author (MP) using predefined search terms (Supplementary Table 1).
Selection of Evidence
The concept and design of the review was undertaken by two authors (MP and MAR). One author (MP) conducted the searching of databases in April 2023, employing referencing system EndNote (version X9.3.3; Clarivate) to manage and categorise searches and articles. Two authors (MP and CT) independently screened identified titles, abstracts and full text articles for eligibility, reaching consensus regarding review inclusion with any disagreements adjudicated by a third author (MAR).
Hand-searching of included articles’ reference lists was undertaken by one author (MP), as was a hand search of the excluded review articles’ references, and the above process repeated for any papers detected via hand-searching.
Data charting of included articles was conducted by one author (MP) and validated by two others (AC and MAR). One author (MP) was responsible for contacting the authors of any papers requiring clarification. All authors approved the final manuscript.
Data Charting
Once consensus had been reached among reviewing authors on included articles, and thus addressed the primary aim, articles were then combed for study outcomes and recorded risk factors.
Data were charted on a standardised table designed for this study using Excel. Mapping of the reported items was also conducted to assist in data organisation (Supplementary Table 2).
Critical Appraisal
A critical appraisal of the included articles was undertaken using the Mixed Methods Appraisal Tool by the first author (MP).23 A second author (AC) appraised a selection of articles to ensure consistency and consensus; even so, this is a subjective application of the tool by the authors.
Synthesis of Results
A summary of all studies that met the inclusion criteria is shown in Supplementary Table 3. Their statistically significant and major findings relevant to the aims of the scoping review were summarised and reported where available.
Results
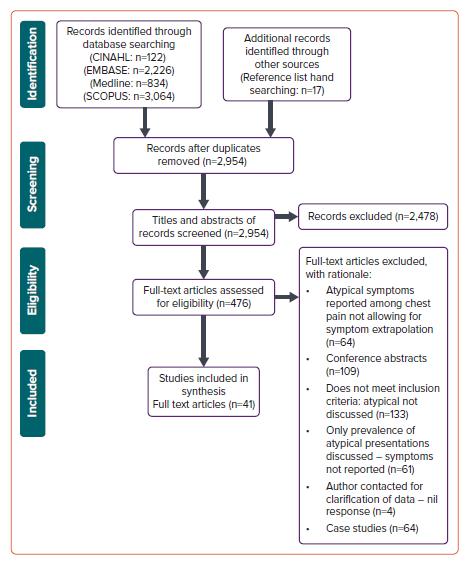
Of the total 2,954 records identified in the search, 41 discussed symptoms of atypical chest pain and/or anginal equivalent presentations across the ACS spectrum and were included in the final analysis (Figure 1). This included all ACS combined (n=12), STEMI (n=13), NSTEMI (n=2), pooled MI (both STEMI and NSTEMI, not separated; n=13) and UA (n=1). Thirty-four articles reported main presenting symptoms only, while the remainder (n=7) combined all symptoms reported by participants (so exceeded 100%), rendering overall symptom frequency analysis implausible (Supplementary Table 2).
Publication dates of articles included spanned 2000–23, with data collection periods from 1993 to 2019 (where reported). Critical appraisal of the included articles employing the mixed methods appraisal tool (MMAT) showed quality was mixed, although a majority scored well: 32 studies (78%) scored 5/5; seven (17.1%) scored 3/5; one scored 2/5 (2.4%); and one 0/5 (2.4%; Supplementary Table 4).23
Definitions and Prevalence: Aim 1
To contextualise results, operational definitions of what constituted a typical or atypical presentation were extracted. Definitions were mixed and varied, with some providing clear definitions while others gave none, leaving their findings open to interpretation (Supplementary Table 3); some gave specified descriptors, locations and pain duration time frames, while others did not. Similarly, what constituted a major adverse cardiovascular event varied between studies.
Included articles predominately dichotomised symptoms into chest pain and non-chest pain (n=27/41), so did not present data on atypical chest pain. Six articles noted pain with or without radiation into the arm as a criterion for a typical presentation; however, four of those specified the left arm.24-29 Additionally, Coronado et al. reported painful versus painless presentations irrespective of pain location, severity or duration, while Gajanan et al. defined ‘any upper body discomfort’ as typical.30,31 Similarly, Gupta et al. assigned patients who presented with any complaint of pain, discomfort or pressure in the chest, left arm/shoulder, jaw or neck into the chest pain category. The remaining articles (n=10) separated atypical chest pain from typical chest pain, along with other listed clinical symptoms that were neither typical nor atypical chest pain, i.e. anginal equivalents.24
Conversely, Ng et al. define typical chest pain as having at least two of central chest pain, radiation to arm or neck, diaphoresis, associated with exertion or documented as ‘cardiac sounding’.32 Moreover, Gajanan et al. included shortness of breath as a typical symptom, independent of chest pain and dyspnoea as an atypical symptom.31 A few specified the inclusion of right-sided chest pain in the typical category, while Lankamali et al. specified a typical presentation as chest pain in the centre or left precordium with or without radiation to the left arm and or both sides of the neck or jaw, and atypical presentation as that involving chest pain in areas other than the above or not accompanied by chest pain.9,27,33
With regards to time frames, three articles specified typical chest pain lasted >20 minutes, one study stipulated chest pain of >30 minutes, while the majority of papers did not specify a time duration as typical.25,29,34,35 It was unclear what occurred with participants who may have experienced pain but of a duration less than those specified – whether they were excluded, considered atypical or other. El-Menyar et al. did not provide a time frame, but defined atypical as not severe, not prolonged or not typical in nature and placed those presenting with dyspnoea as one of three separate groups (typical symptoms of myocardial ischaemia; atypical chest pain; and dyspnoea) during their analyses, excluding other anginal equivalents (e.g. loss of consciousness, palpitation, generalised body aches, becoming fatigued easily or epigastric discomfort) that formed a small minority of the entire sample.26
Among articles that dichotomised symptoms into chest pain and nonchest pain cohorts, the proportion of anginal equivalent presentations was wide-ranging, going from 3.9% to 59%.36,37 Where symptoms of typical chest pain were separated from atypical chest pain and other anginal equivalents, atypical symptom presentation (including atypical chest pain) was in a range of 10%–57%.29,31 Some authors noted cardiac arrest as an atypical symptom, Taylor et al. identified it as a typical presentation and others noted it as a criterion for exclusion.9,11,24,26,30,33,34,36,38–44
Of all the articles that combined acute MI types, only one article separated STEMI and NSTEMI symptomology, while another published findings on combined acute MI in 2016 then in 2019, conducted a sub–analysis of their NSTEMI cohort and published those findings including symptom proportions.45–47 Eleven articles explored symptoms of ACS patients as a group (nil differentiated symptoms by ACS type), and only one article exclusively studied UA patients.9
Atypical Chest Pain and Anginal Equivalent Symptoms: Aim 2
Dyspnoea was the most reported symptom across all included articles (n=39/41). Of those 39 studies, 29 reported dyspnoea as the most prevalent anginal equivalent, in a range of 11.2%–72% of presentations, with another two reporting dyspnoea sharing the highest position with another: syncope and fainting/falling.30,37,40,44
Similarly, neurological symptoms were commonly investigated (n=28/41), encompassing: loss of consciousness, syncope, presyncope, collapse, faint and unconsciousness, which varied from 4.1% to 36.4% of presentations.35,44 These were sometimes collated and reported separately at other times.11,24,32,33,37,46,47 Fatigue, weakness or lethargy also accounted for high proportions of presentations, spanning 4.3%– 60% across 15/41 studies; when investigated, atypical chest pain (n=12/41), also described as non-specific, pleuritic or burning, was another common symptom, reported in 11.1%–72%.29,32,42,48 Nausea and vomiting were also identified with high frequency (n=21/41) and proportion (range 1.7%–25.8%) although, again, were reported as distinct symptoms, combined or consolidated as gastrointestinal symptoms.9,11,s24,28,33,35,37,40–45,49–55 Notably, diaphoresis (including sweating, clammy skin and perspiration) featured in 12/41 studies in a reported range of 2.4%–27.9%.49,54
Pain or discomfort in the neck, jaw, shoulder and arm were often combined in various permutations. When examined as its own entity and not a condition of a typical presentation, arm pain was reported by five articles.9,33,45,52,55 Three of these stated arm pain, one reported pain in the left and right arms separately (10.3 and 0.9%, respectively) and one mentioned the left arm alone (5.1%).9,33,45,52,55 Pain in the shoulder, neck and jaw was not overly subjected to left- and right-sided differentiation. See Supplementary Table 5 for a full list of symptoms and proportions. Other symptoms less commonly reported included (though not exclusively) cardiac arrest, diarrhoea, cough, hiccups, headache, indigestion and altered mental status (Supplementary Table 6).
Risk Factors: Aim 3
Of all the included articles, 28/41 reported common cardiovascular disease risk factors frequently hypothesised to be a predictor of ACS presentation without cardiac chest pain. Those included advanced age – noting, however, that the age range of included participants across all studies was in a range of 55–85 years, so advanced age was variously defined – female sex, numerous relevant comorbid conditions and prior medical events (Supplementary Table 7).
Of the demographic characteristics reported, the most frequent were sex and age (n=22/28 each). Evidence for higher rates in women was mixed. Thirteen studies reported a positive (un)adjusted association, i.e. unadjusted and adjusted associations inclusively.11,24,26,28,29,34,36,37,42,44,54,56,57 The remaining nine studies did not.9,27,30,33,41,43,47,48,58 The relationship between age and presentation without cardiac chest pain was clearer, with 17/22 studies showing a positive (un)adjusted association,9,11,24,28,30,34,41–44,46,47,53,54,56,58,59 and five failing to do this (Supplementary Table 7).26,27,29,37,48
Pertaining to comorbid conditions, diabetes was the most reported (n=18/28). Seven studies found an (un)adjusted association.11,26,28,29,34,44,56 However, the majority (n=11/28) did not.9,27,30,33,37,42,43,47,48,54,58 Seven studies reported a negative (un)adjusted association between atypical presentation and smoking.11,26,28,34,42,44,56 Nonetheless, seven did not.9,27,29,43,47,48,58
Yet again, vast heterogeneity was present regarding variables of interest and statistical methods employed (Supplementary Table 7). Hwang et al. and Grosmaitre et al. pooled different comorbid pathologies to report them in combination.37,58 Coventry et al. reported mixed adjusted results across age categories, and Hwang et al. examined differences in atypical presentations between old and young and so found combined associations across cohorts (i.e. comorbid conditions, dyslipidaemia and diabetes).33,58 Similarly, Borden et al. and Gupta et al. had mixed results on ethnicity, with some ethnicities more likely to present without cardiac chest pain.24,48
Outcomes: Aim 4
Of the 41 included articles, 24 reported on any of the outcomes pertinent to the final aim of this scoping review, namely mortality, heart failure (HF) and major adverse cardiovascular events, delays, diagnosis and medical interventions (Supplementary Table 3).
Overall outcomes for ACS presentations without cardiac chest pain were overwhelmingly poor. Articles that reported on death unanimously reported higher mortality rates with the exception of one paper examining UA at univariate analysis, and another examining pooled ACS at multivariate analysis.9,37 Patients without cardiac chest pain consistently had higher rates and severity of HF (reported as either HF on presentation or via Killip class) with or without major adverse cardiovascular event, delayed first medical contact/hospital presentation from symptom onset, longer ECG acquisition and door-to-balloon times, reduced guideline adherence including regarding medication administration during admission and at discharge,with the exception of angiotensin-converting enzyme inhibitors in two studies.9,11,26,28,30,34,37,42–44,47,48,52,54,56,58 They were less likely to undergo cardiac interventions (including coronary angiography, coronary artery bypass graft and percutaneous coronary intervention) when indicated, were less likely to be admitted to a unit providing higher care (i.e. intensive care or cardiac care unit) and had longer stays in hospital (6.0–6.6 versus 4.2–5.0 days).9,11,26,28,30,33,34,37,42– 44,47,54,56,58,60 They were also less likely to be diagnosed with STEMI.26–28,33,54,56,58
Discussion
ACS patients presenting without cardiac chest pain were poorly understood and ill-defined, posing significant challenges for recognition by patients as well as clinicians. While cardiac chest pain remains a heralding symptom, mounting evidence suggests other symptoms may indicate ACS, of which clinicians should be aware.7 This review collated available evidence for the first time not only to understand symptomology beyond cardiac chest pain but also to examine risk factors and outcomes for these patients.
Experts in the field have repeatedly called for standardised definitions as well as collection and reporting standardisations – this scoping review has illuminated the extent of this need, with meta-analysis of data implausible due to the vast heterogeneity.61 Recent advancements within the past 2 years in the American Heart Association/American College of Cardiology guidelines on chest pain evaluation and diagnosis, as well as in their guideline on key data elements and definitions for chest pain and acute MI, have provided a platform to address this; these should be adopted going forward to facilitate consistency in clinical practice and reporting, translating to a better understanding of this cohort.14,15 Data for the present review were collected before these guidelines were published and, therefore, included studies that do not reflect their recommendations. Nonetheless, the terms cardiac chest pain and anginal equivalents should be embraced in both clinical and academic settings to reduce ambiguity and close the outcome discrepancy gap.
Despite overwhelming heterogeneity in operational definitions, data collection methods, inclusion/exclusion criteria and reported variables across all included studies, the consistent theme of significantly poorer outcomes in patients without cardiac chest pain was stark. These included higher mortality rates in both the short and the long term, greater severity of HF, delayed presentation to first medical contact, less guideline-driven care and higher rates of misdiagnosis. This is consistent with other studies, including the large SWEDEHEART registry (n=172,981).62,63
Symptomology is one of the three main criteria (along with biomarker assays and ECG) that inform a clinical diagnosis of ACS.64 Clinical judgement and decision-making are underpinned by pattern recognition, including regarding symptoms and their degree of pathognomicity.65 Consequently, vague symptoms or a lack of a typical pattern – or an ambiguous pattern presentation – have consistently been linked to cognitive errors and misdiagnosis, with Brieger et al. finding a 10-fold incidence of misdiagnosis, which may partially explain the worse outcomes observed.11,66
Despite its limited prognostic value, chest pain is associated with improved patient prognosis including overall outcomes.67 This is presumably owing to anginal equivalents or, indeed, mild chest pain presentations being erroneously misinterpreted as having a lower disease burden, with severe chest pain presentations afforded higher clinical relevance and consequently receiving investigations with greater expediency and vigour.67 Outcome discrepancies between those with chest pain and those without disappear when both are addressed equitably with regards to ECG acquisition and catheterisation laboratory intervention, which emphasises the importance of early recognition.13,48
Our review highlights that discharge medication regimens and cardiology follow-up, including cardiac rehabilitation, were less likely among patients without cardiac chest pain compared to those with, suggesting that, even after an ACS diagnosis is reached, these patients still receive suboptimal care. This requires additional investigation – and may also reflect the fallaciously lower perceived level of disease burden.
Our findings demonstrate that regarding symptoms aside from chest pain, dyspnoea appears important. A study by Pope et al. discovered that, among acute MI patients, a chief symptom of dyspnoea was a significant contributing factor for inappropriate discharge from the emergency department.68 The Acute Coronary Syndrome Israeli Survey revealed that, in the setting of chest pain and without signs of HF, those who also experienced dyspnoea had statistically significantly worse outcomes and were more likely to report atypical chest pain (14% versus 6%; p<0.001).69
While atypical chest pain clearly featured in this review, numerous articles examined chest pain/no chest pain as a dichotomous variable. This approach neglects chest pain descriptors as well as other pain characteristics including severity and location. Contemporary guidelines acknowledge descriptors such as sharp and pleuritic have a low index of suspicion of an ischaemic aetiology; however, they are still noted as a permissible value and, therefore, should be investigated accordingly.15,70
Furthermore, research by Goodacre et al. reported radiation to shoulder and both arms was a predictor of acute MI at multivariate analysis (OR 5.7; 95% CI [1.5–21.4]; OR 4.9; 95% CI [1.3–19.4]; respectively), but radiation to the left arm or right arm was not significant. They concluded that many commonly used clinical features failed to show association with acute MI or ACS diagnosis.71
Other factors that are commonly associated with presentations without cardiac chest pain include female sex and comorbidities, such as diabetes, HF and hypertension; this review found a lack of consistent evidence to confirm these assumptions.
While female sex is often linked with atypical ACS presentation, the present review found just under half of studies supported this. However, when adjusted for confounders, only a small proportion found female sex to be an independent predictor.36 Conversely, and as expected, advancing age was frequently found to be an independent factor. A cause for the former assertion that sex is related to presentation may be attributed to women presenting at an older age with ACS than men, which may account for the association being lost after adjustments for confounding variables, such as age, have been made.72 This is consistent with a review conducted by Canto et al. in 2007 that previewed the literature from 1970 to 2005, which proclaimed older age was a greater consequential predictor than sex for presentations without cardiac chest pain.73 These findings are also similar to a systematic review and meta-analysis by Coventry et al., which showed women had lower odds of presenting with chest pain; however, significance was retained in only three of the five included studies that adjusted for age.74 Arguably, both women and men report chest pain, but differences in proportions of symptoms have been observed in the literature, with women experiencing more ACS-related symptoms and with greater severity and symptom burden as well as having more modifiable risk factors.36,39,72,75–77
Diabetes has been hypothesised to be related to presentations without cardiac chest pain due to changes in pain perception likely due to neuropathy.78 Where the relationship of age was strong, despite diabetes often touted as a predisposing risk factor for atypical ACS presentation, the findings from this review challenge this stance – both at unadjusted and adjusted levels. Where other comorbid conditions, such as hypertension, dyslipidaemia and renal disease, have also previously been considered important, this review highlights the need for further research using multivariate analysis with proper adjustment for confounders to further explore direct association, rather than proportions; this was lacking across most studies, making direct conclusions difficult. Smoking status inferred a negative association but, again, this was subject to the limitations mentioned above. Previous HF, family history of vascular disease as well as previous cardiovascular disease-related events yielded mixed results across studies (Supplementary Table 7).
This review highlights that the current status of evidence is plagued by inconsistencies, largely owing to a previous lack of a standardised definition of symptoms extending from cardiac chest discomfort and a lack of reporting guidelines that would otherwise facilitate consistency in data collection, analysis and interpretation. New guidelines offer a prospect of this occurring in future research. In the studies reviewed, there was heterogeneity and inconsistency among methodologies, definitions of atypical including descriptors, various time frames (if present), chief symptom versus all symptoms as well as the use of synonyms, for example, collapse versus (pre)syncope used with no clear explanation. Inconsistent inclusion and exclusion criteria were evident, for example cardiac arrest, as mentioned. The type of MI was not explicated in many studies (i.e. type 1 versus type 2) and therefore we were unable to identify whether differing pathologies yield differing symptoms.
Clinical and Research Implications
Where outcomes for ACS patients have largely improved latterly, this does not hold true for patients presenting without cardiac chest pain. It is anticipated that, with a clearer understanding of these patients’ clinical pictures, easier identification would follow, and accordingly, appropriate treatment would reduce present outcome gaps between those presenting with cardiac chest pain versus those without. This will subsequently help inform community awareness programmes and campaigns, reduce prehospital delay, support prehospital providers to determine appropriate hospital destination with cardiac capabilities and assist in appropriate nursing triage and clinician treatment pathways.
This must extend to beyond merely raising awareness of different symptoms to discharge care regimens such as prescribed medications, cardiology follow-ups and rehabilitation.
Before this can fully occur, adoption of recent guideline recommendations regarding the evaluation and diagnosis of chest pain, as well as adherence to the clinical data standards outlined, should be undertaken by clinicians and researchers to facilitate accurate data collection, analysis and interpretation.
Our current understanding is that mortality and morbidity are significantly greater in those presenting without typical chest pain, so the need is pressing and substantial.
Strengths and Limitations
This review is one of the first studies to collate symptoms reported across ACS patients not presenting with cardiac chest pain, as well as their outcomes, risk factors and definitions used. Scoping reviews are subject to limitations and some articles may have been missed; however, the search and reporting were approached in a systematic way to mitigate this.
Throughout the process, it was discovered that the present literature does not support a systematic review because of its substantial heterogeneity; therefore, it does not facilitate meta-analyses. We were unable to pool results from studies or apply statistical analyses and have subsequently tabulated findings from this research; many of the claims made are descriptive. However, this was not our objective as we primarily sought to identify symptoms other than cardiac chest pain and their proportions reported among ACS patients, and include risk factors and outcomes for that cohort. This review sought to canvas the literature, though the opportunity to conduct systematic reviews and meta-analyses with more targeted objectives – including outcomes resulting from specific presentation types – should be possible in future, if recommended terminology and definitions around symptoms are adopted and participants better defined.
Another limitation is the exclusion of non-English articles, case studies and grey literature, potentially neglecting emerging findings that may be under-reported in published or English language literature.
Conclusion
This paper summarises the atypical chest pain and anginal equivalent symptoms reported throughout the literature since 2000. It also summarises the outcomes experienced by patients presenting without cardiac chest pain as well as the risk factors for these presentations; while chest pain is a predominant and cardinal symptom of ACS, it is far from pathognomonic.
This paper offers a critical starting point for understanding presentations without cardiac chest pain better, and encourages standardised data gathering and reporting, lending support to the adoption of recent guidelines. This will facilitate greater understanding of this cohort and early identification, translating to better patient outcomes, reduced misdiagnosis and enhanced clinical decisions. All of these foster equality of care whether patients are presenting with chest pain or other symptoms. Until this is realised, current clinical assumptions such as female sex, certain comorbid conditions and previous cardiovascular events should be challenged, with this review disseminating the importance of advancing age and potential symptoms clinicians should not underestimate.