Women have a poorer prognosis following ST-elevation MI (STEMI) than men.1–7 Although sex-based differences in post-STEMI outcome are well documented, the reasons for these poorer outcomes in women are less well defined, which limits our ability to close this sex-based outcome gap. The role played by differences in the anatomical complexity of coronary artery disease or by multivessel disease (MVD) in sex-based outcome differences at long-term follow-up is not well established. There is an increasing recognition of the prognostic importance of MVD and incomplete revascularisation, but there is a paucity of data evaluating the degree to which sex-related differences in MVD and incomplete revascularisation perpetuate sex-based outcome disparities or persist over time.2,7–13 Recent studies have shown that women less frequently receive revascularisation and optimal medical therapy.2–4 A number of studies have demonstrated that in STEMI cohorts sex differences remain significant after multivariable risk adjustment, but many studies depend on relatively short follow-up periods of 30 days–6 months.1–7,14 To evaluate associations between sex, MVD, incomplete revascularisation, prescribing practices and early and late outcomes after STEMI we compared rates of cardiac death and MI between women and men with single-vessel disease (SVD) and MVD in a large cohort of consecutive percutaneous coronary intervention (PCI)-treated STEMI patients.
Methods
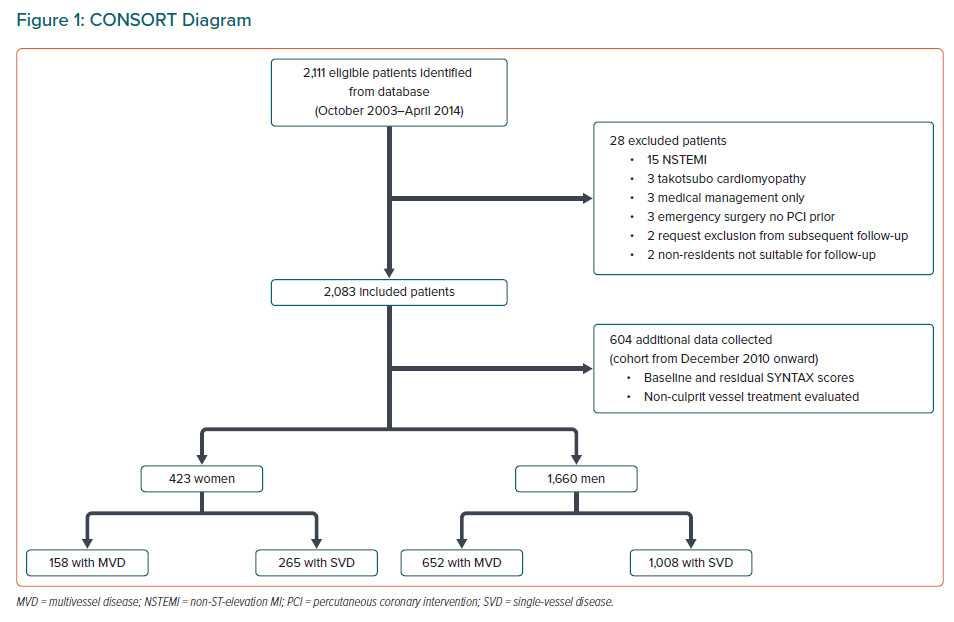
To evaluate sex-based differences in rates of cardiac death and MI between those with SVD and MVD from October 2003 to April 2014 a consecutive cohort of patients presenting with ST elevation treated with PCI during index hospitalisation from five Australian hospitals were studied as previously described.15 A CONSORT diagram is shown in Figure 1. Patients were included if treated with primary PCI, rescue PCI, or successful fibrinolysis followed by prognostic PCI. Patients with left main coronary artery (LMCA) stenosis, chronic total occlusion and cardiogenic shock were also included. Patients who received medical management only for their STEMI and those treated with urgent coronary artery bypass graft surgery without initial PCI were excluded (Figure 1). Ethics approval for clinical follow-up including direct patient contact was obtained from the Southwest Sydney Local Health District Human Research Ethics Committee (QA08/034), and all research activity was performed in accordance with the Declaration of Helsinki.
Angiographic, procedural and clinical data were prospectively collected as previously described.15 Long-term follow-up information was collected by contacting cardiologists, general practitioners, or patients/next of kin, and included a review of medical records, outpatient letters and laboratory results. A day 7 time point for events was also included in results, given that most outpatient staging would occur at >7 days, and most inpatient staging would be completed within 7 days of the primary event. This was to enable readers to hypothesise about or assess the potential impact of deferring non-culprit PCI to outpatient care. In patients from 2010 onwards the SYNTAX scores were calculated, and prescribing practices were included in captured data. Treatment decisions were made by the interventional cardiologist and/or attending consultant.
STEMI was defined as chest pain of ≥30 minutes’ duration and persistent ST-segment elevation ≥1 mm in two contiguous leads (or ≥2 mm in V2–V3) or new left bundle branch block with associated elevation in troponin T. MVD was defined as ≥70% stenosis in ≥2 major epicardial vessels; patients with LMCA stenosis ≥50% were also included in this definition. Sex was defined using patient-supplied information. Definitions for cardiogenic shock, diabetes, hypertension, smoking status, renal impairment and lesion complexity were defined as previously described, as were death, cardiac death, MI, target vessel revascularisation and definite stent thrombosis.15
Continuous variables are given as median and IQR for non-Gaussian variables and as the mean and standard deviation for Gaussian variables, and variables were compared using the Kruskal–Wallis test or two-sample t-tests as appropriate. Categorical variables are summarised as frequencies and percentages and were compared using the chi-squared test or Fisher’s exact test, as appropriate. Time-to-event outcomes were followed for events of interest; time was commenced at admission for STEMI; patients were censored at the time of last follow-up, and Kaplan–Meier analysis was performed. Cox proportional hazards models were used to calculate HR and 95% CI. Cox proportional hazards multivariable modelling was performed for the primary and secondary endpoints. The nine factors considered in the model were age, sex, diabetes, renal dysfunction, cardiogenic shock, culprit LAD lesion, MVD, dyslipidaemia and hypertension at index hospitalisation based on previous studies.4,12,15–17 In order to assess the proportional hazards assumptions in Cox regression analyses, global score tests were performed, and the proportional hazards assumption was met for the final model. A two-tailed p-value ≤0.05 was considered statistically significant, and no adjustments have been made for multiple comparisons. SPSS Statistics, v21.0, SAS v9.4 and Stata v12 were used for analyses.
Results
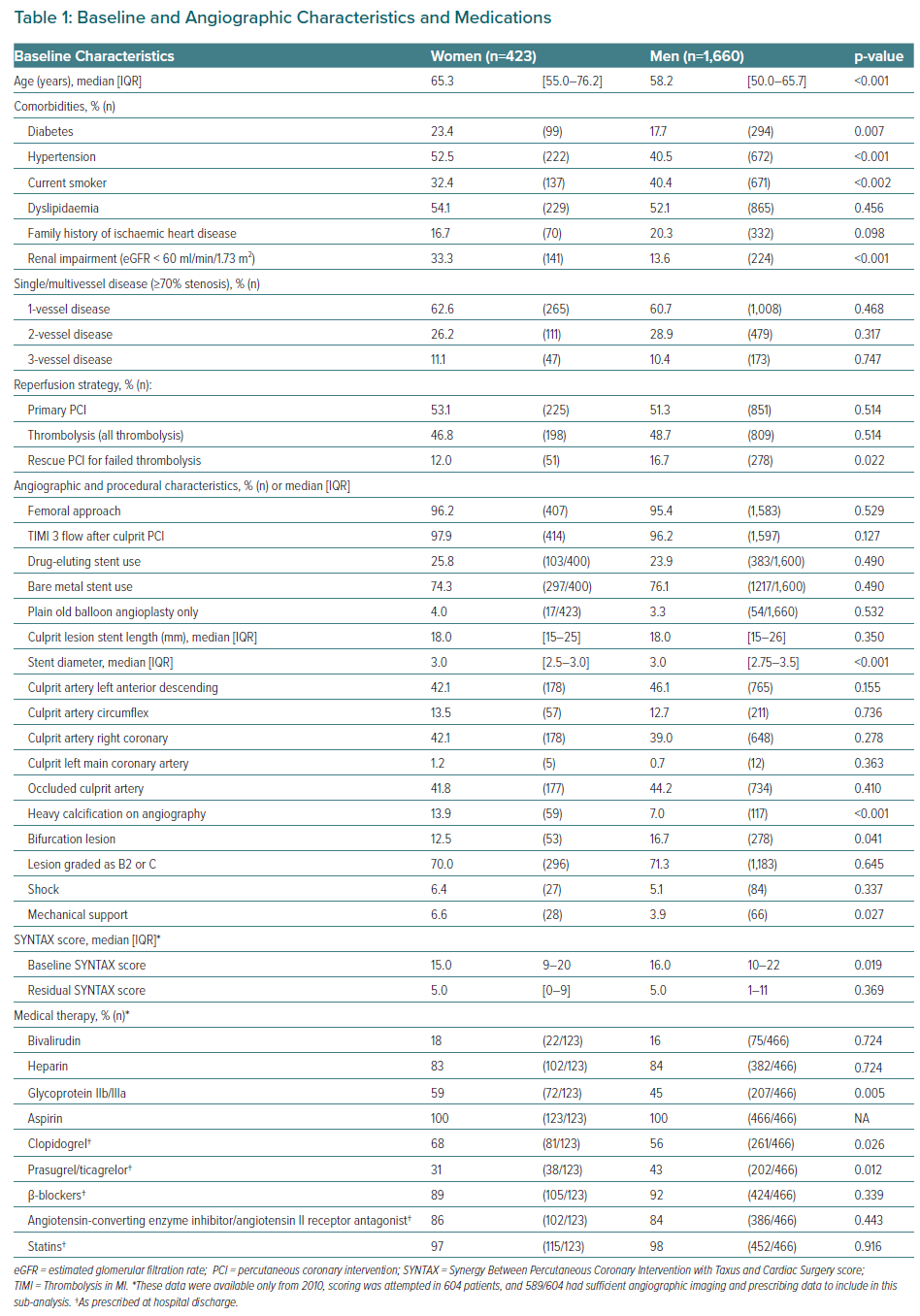
Of the 2,083 STEMI patients included in this consecutive STEMI cohort, 20.3% (423/2,083) were women and 79.7% (1,660/2,083) were men. There were no differences in the rates of primary PCI or fibrinolysis between women and men (Table 1). However, a smaller proportion of women received rescue PCI following fibrinolytic therapy than men: 12% (51/423) versus 16.7% (278/1,660; p=0.022). Women, when compared with men, were older and were more likely to have diabetes, hypertension and renal impairment, but were less likely to be smokers (Table 1).
Procedural characteristics were similar between groups (Table 1). MVD was present in 36.9% (156/423) of women and 39.3% (652/1,660) of men (p=0.468). From 2010, SYNTAX data, prescribed medical therapy data and data detailing elective non-culprit vessel treatment were collected (Table 1). A lower proportion of women received guideline-directed potent P2Y12 inhibitors (ticagrelor and prasugrel) than men (31% versus 43%, p=0.012), particularly patients with MVD (25% versus 45%; p=0.011). At presentation women had a lower burden of coronary artery disease than men: the median baseline SYNTAX score was 15.0 (IQR [9–20]) in women and 16.0 (IQR [1–11]) in men (p=0.019). On completion of all planned non-culprit procedures, the median residual SYNTAX scores (rSS) did not differ between sexes, and it was 5.0 (IQR [0–9]) in women and 5.0 (IQR [1–11]) in men (p=0.369). In patients with MVD, the median rSS was 9 (IQR [6–17]) in women, and 10 in men (IQR [6–15]; p=0.838). Using SYNTAX-based definitions for complete revascularisation, in patients with SYNTAX score data 33% of women and 44% of men with MVD achieved rSS<8 (p=0.401), and 4% of women with MVD and 3% of men with MVD achieved an rSS=0 (p=0.584).
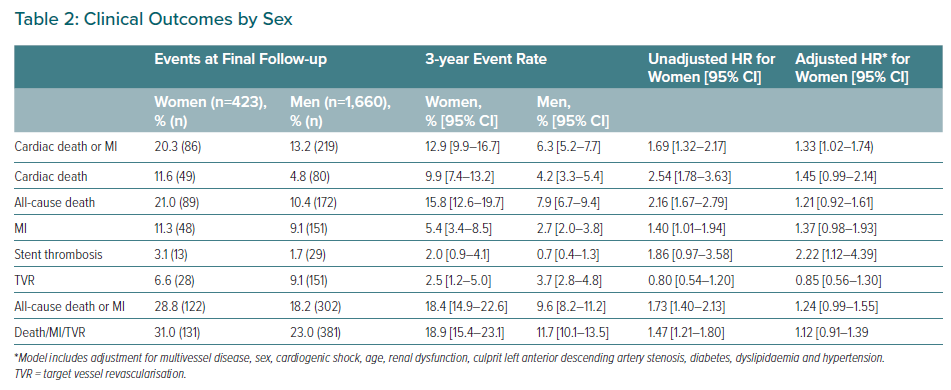
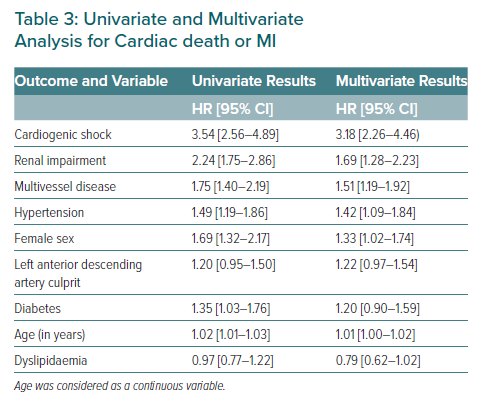
The primary outcome of cardiac death or MI occurred in 14.6% of patients (305/2,083) at final follow-up (median 3.6 years; IQR [2.4–5.4]), with follow-up of ≥6 months in 2,036/2,083 patients (97.7%) and ≥1 year in 1984/2,083 (95.0%). Cardiac death or MI occurred more frequently in women (20.3%, 86/423) than men (13.2%, 219/1,660; p=0.028), with 3-year event rates of 12.9% (9.9–16.7) in women and 6.3% (5.2–7.7) in men (p=0.035). Female sex was associated with an increased rate of cardiac death or MI on univariate (HR 1.69; 95% CI [1.32–2.17]) and multivariate analysis (adjusted HR [aHR] 1.33; 95% CI [1.02–1.74]; Table 3).
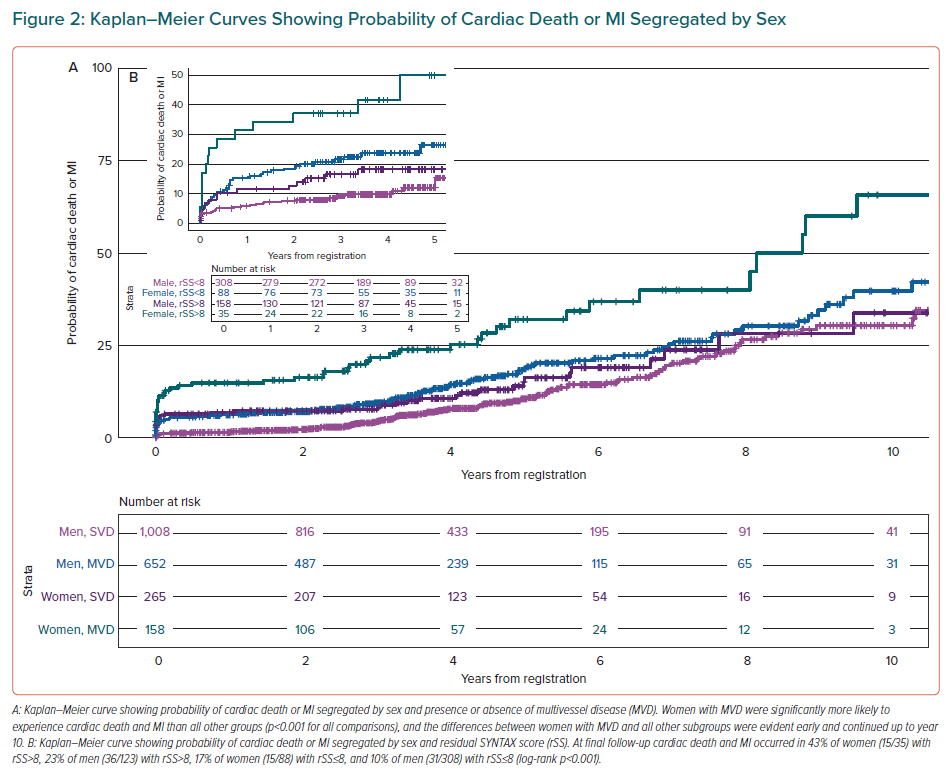
When divided into four groups by sex and MVD status, Kaplan–Meier analysis indicated significant outcome differences. Women with MVD were significantly more likely to experience cardiac death and MI than all other subgroups (p<0.001 for all comparisons), and differences between women with MVD and all other subgroups were evident within 7 days and continued up to year 10 (Table 2; Figure 2A).
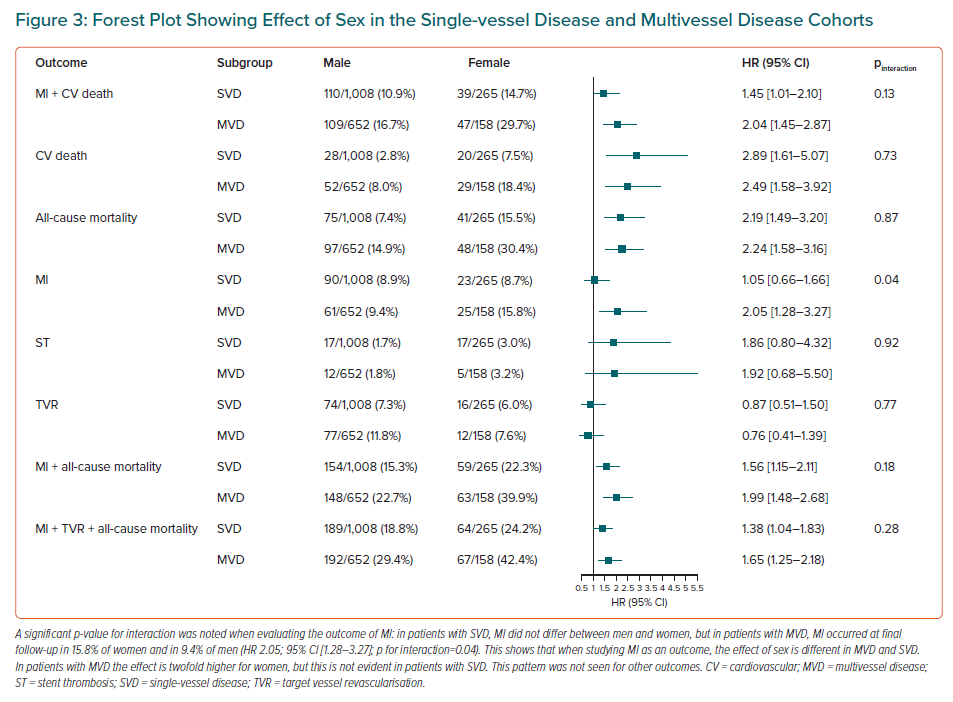
At final follow-up in patients with MVD, cardiac death or MI occurred more frequently in women (29.7%, 47/158) than men (16.7%, 109/652; HR 2.04; 95% CI [1.45–2.87]); 3-year cardiac death or MI rates were 21.8% in women with MVD and 9.5% in men with MVD (p<0.001). In patients with SVD, cardiac death or MI occurred at final follow-up in 14.7% of women (39/265) compared with 10.9% of men (110/1008; HR 1.45; 95% CI [1.01–2.10]), with 3-year event rates of 7.8% in women with SVD and 4.3% in men with SVD (p=0.046; Figure 3).
At day 7, 7.6% of women (12/158) with MVD had experienced cardiac death or repeat MI compared with 3.7% of men (24/652) with MVD (p=0.032) and 3.8% of women (10/265) with SVD (p=0.087). Women with SVD at day 7 had rates of cardiac death or MI of 3.8% (10/265) compared with 0.5% in men with SVD (5/1,008; p<0.001). Outcomes for all secondary endpoints are listed in Table 2.
In the cohort from 2010 onward, 589 of 604 patients had imaging enabling SYNTAX scores to be evaluated. Women with rSS>8 were significantly more likely to experience cardiac death and MI than all other groups, (p<0.001 for all comparisons; Figure 2B). Kaplan–Meier analysis indicated sex-based outcome differences (Figure 2B). When divided into four groups by sex and rSS, cardiac death or MI occurred in 43% of women (15/35) with rSS>8 and 23% of men (36/158) with rSS>8 (HR 2.14; 95% CI [1.17–3.91]; p=0.01), and occurred in 17% of women (15/88) with rSS 0–8, and 10% of men with rSS 0–8 (31/308; HR 1.68; 95% CI [0.91–3.12]; p=0.10; pinteraction=0.58).
Discussion
This study has found higher rates of cardiac death or MI in women compared with men in patients with STEMI undergoing PCI with long-term follow-up. These differences remained significant following multivariable risk-adjusted analysis, adjusting for age, comorbidities, acuity of presentation, MVD and infarct site. Sex-based differences were predominantly found in patients with MVD and in patients with a high burden of incomplete revascularisation. Data from this study also showed that differences in rates of cardiac death or MI between women and men were evident within 7 days and continued to diverge years into late follow-up. Differences persisted following multivariate risk adjustment. Women in this consecutive cohort of STEMI patients were not found to have higher rates of MVD or higher rSS on completion of all planned procedures than men. However, Kaplan–Meier analysis found that sex-based differences in rates of cardiac death or MI were predominantly evident in patients with MVD and with a high burden of incomplete revascularisation. After 8 years, one in every two women with MVD and STEMI had experienced cardiac death or MI, close to double that of men with MVD, women with SVD, and men with SVD. Differences in rates of cardiac death or MI between these subgroups were also seen early and were significant within 7 days of the initial STEMI, suggesting that the best time to initiate management strategies to mitigate current sex-based outcome differences may be in the first days post-MI, not weeks or months.
Data also suggested that differences in prescribing practices for these patients may explain some of these outcome disparities. In the present study, particularly in patients with MVD, significantly more men than women received potent P2Y12 receptor inhibitors. However, our findings related to P2Y12 prescribing and sex are hypothesis-generating and require further validation in a larger cohort; available data in this cohort are not sufficient to unequivocally validate these observations. These findings strongly suggest that studies evaluating sex-based outcome differences should also report any sex-based differences in the prescription of potent P2Y12 receptor inhibitors, given that differences in P2Y12 prescribing practices may contribute to poor outcomes for women with MVD and incomplete revascularisation.
The significantly higher rates of cardiac death and MI found in women on both univariate analysis and multivariate risk-adjusted analysis observed in this study are in keeping with other contemporary analyses of large STEMI cohorts reporting shorter-term outcomes. A number of studies reporting short-term outcomes found that sex-based differences remain significant after multivariable analysis including age.1–4,6,7,14,18 Heer et al. published a large observational study of primary PCI-treated STEMI patients (n=185,312) evaluating in-hospital outcomes and found, after multivariable analysis including age, that women were 1.19-fold more likely to die in hospital than men (95% CI [1.06–1.33]).1 Stehli et al. analysed Victorian Cardiac Outcomes Registry (VICOR) data from 5,749 STEMI patients who underwent PCI and found, after multivariable analysis including age, that women were 1.67-fold more likely than men to die at 30 days (95% CI [1.11–2.49]).3 Khan et al. analysed CONCORDANCE (Cooperative National Registry of Acute Coronary care, Guideline Adherence and Clinical Events) data, involving 41 Australian and New Zealand hospitals (n=2,898), studying all acute coronary syndrome (ACS) patients including those not offered angiography or revascularisation, found, after multivariable analysis including age, that women were 2·17-fold more likely to die after STEMI than men (95% CI [1.24–3.80]) at 6-month follow-up.4 A large meta-analysis by Pancholy et al., which included 68,536 STEMI patients treated with primary PCI, found that in-hospital mortality was significantly higher in women compared with men after multivariable risk adjustment (RR 1.48; 95% CI [1.07–2.05]), but noted that this risk-adjusted difference was no longer significant at 1 year.5 However, Kvakkestad et al. found no significant mortality difference at 5 years between sexes after multivariate analysis in 5,159 consecutive Norwegian STEMI patients (2005–2011), including those not offered angiography or revascularisation in the era prior to widespread use of potent P2Y12 inhibitors (ticagrelor or prasugrel).19,20 Pooled data for all acute MI are more heterogenous, suggesting the importance of evaluating data for STEMI cohorts separately.1,21,22 We note that most studies evaluating sex differences do not include incomplete revascularisation or MVD status in risk adjustment models and usually report all-cause mortality data, rather than the endpoints of cardiac death or cardiac death and MI. By evaluating these factors the present study provides new insights and hypotheses regarding the drivers of these sex-based differences and suggests that targeting prescribing practices and the completeness of revascularisation in those with MVD may help to close the outcome gap for women with STEMI.
Our study (n=2,083) did find significant sex-based differences in cardiac death and MI before and after risk adjustment at long-term follow-up. After risk adjustment, sex-based differences in rates of cardiac death alone became only a trend (Table 2). The univariate HR for cardiac death was 2.54 (95% CI [1.78–3.63]) but became non-significant using this model (HR 1.45; 95% CI [0.99–2.14]). This differs from other studies.1,3–5 This issue is likely to be related to power and cohort size. A larger patient cohort, as evaluated by Heer et al., Stehli et al., Khan et al. and Pancholy et al., may be required to demonstrate sex-based cardiac mortality differences in PCI-treated STEMI patients.1,3–5
This study also suggests that the inclusion of MI as an endpoint may be important when studying sex differences in STEMI patients, especially in view of observed sex-based discrepancies in P2Y12 prescribing practices. In patients with SVD, MI did not differ between men and women; however, in patients with MVD, MI occurred at final follow-up in 15.8% of women and in 9.4% of men (HR 2.05; 95% CI [1.28–3.27]; pinteraction=0.04), suggesting that non-culprit lesions and vessels play a significant role in sex-based outcome discrepancies, which may potentially be at least partially mitigated by more guideline-concordant prescribing practices. This also suggests that strategies based on decreasing MI rates for women with MVD such as timely complete revascularisation may successfully reduce outcome disparities between sexes.
This study also serves as a reminder that when evaluating prescribing practices in STEMI patients, collecting data regarding potent P2Y12 prescription is important. We note that data collected prior to 2010 may not show this, given that potent P2Y12 inhibitor use was endorsed by guidelines only after the Plato trial (2010) was published. Data captured earlier may not reflect sex-based prescription differences given that clopidogrel (a less potent P2Y12 inhibitor) was used in the majority of all ACS patients. In this study, we collected prescription data only in a subgroup of patients (those enrolled from 2010 onward), in part due to the availability of computerised prescribing data. Further research is needed.
We can hypothesise that one of the causes of sex-based differences in the rates of MI may relate to the lower usage of potent guideline-recommended P2Y12 antiplatelet agents in women, particularly in women with MVD. The use of these drugs has been shown to decrease rates of death, MI and stent thrombosis in STEMI patients when compared with clopidogrel, but under-utilisation of these guideline-recommended medications is common.23 In our study significantly more men than women received potent P2Y12 receptor inhibitors, and of those with MVD men were almost twice as likely as women to be prescribed these guideline-recommended drugs. There is evidence that women with STEMI are less likely to receive guideline-based therapy than men, but there are few studies directly linking sex-based outcome disparities with MVD and lower prescription of potent P2Y12 agents as this study does.3,4 Our data collected from 2010 onwards suggest that further investigation into the impact of under-prescription of guideline-recommended potent P2Y12 receptor inhibitors is warranted when addressing sex-based outcome disparities. Stehli et al. report data demonstrating lower rates of ticagrelor prescription (63.5% versus 60.2%, p=0.004), but do not also report rates of prasugrel prescription, or describe rates with MVD.3 Further analysis of data from Olier et al. reporting UK P2Y12 prescribing practices from the British Cardiovascular Interventional Society national database also shows lower rates of prasugrel and ticagrelor prescription for women with STEMI treated with primary PCI (32%, 7,359/22,786) compared with men (35%, 23,460/66,281; p<0.001).24
The impact of incomplete revascularisation should also be considered. Women with a high burden of incomplete revascularisation are twice as likely as men with a high burden of incomplete revascularisation to experience cardiac death or MI after STEMI.2 Incomplete revascularisation may affect outcomes for women to a greater degree than it does for men particularly in the setting of lower rates of prescription of potent P2Y12 receptor inhibitors as observed in this study.2
Limitations
This observational study should be considered primarily hypothesis-generating. It has limitations including the collection of prescribing data and SYNTAX scores only from 2010 onward, and the generalisability to STEMI patients not receiving PCI must also be considered. Power may be limited by cohort size, particularly when assessing differences between subgroups. Given that SYNTAX score data and data regarding medications were collected only from 2010 onwards, these data may also be subject to type 2 errors and could not be included in risk adjustment models. There is no universally accepted definition for complete revascularisation.12,25 As we have noted in previous studies, we favour rSS<8 to define high-risk incomplete revascularisation, but acknowledge that an rSS=0 is numerically more correct.12 We acknowledge that debate may occur regarding the completeness of revascularisation in clinical settings in which some scorable lesions with a negative functional assessment or stenosis of 50–70% are present. The validity of any single definition of completeness of revascularisation may be debated, therefore we have tried where practical to present data for rSS=0 and rSS<8. Significant changes to contemporary practice with respect to drug-eluting stent use, radial access and P2Y12 selection over the study period, and time for late follow-up, and changes to regional systems of STEMI care to improve rural patient access primary PCI are also acknowledged as limitations of this study, as is the proportion of patients who received PCI after thrombolysis. In this study information on bleeding risk and co-prescription of direct oral anticoagulants was not available and limits the interpretation of prescribing decisions.
Conclusion
This study reports a higher incidence of cardiac death or MI in women compared with men, which remains significant after risk adjustment. Female sex (after risk adjustment) was independently associated with cardiac death and MI (aHR 1.33; IQR [1.02–1.74]). This study found that sex-based differences in rates of cardiac death or MI were evident in patients with MVD. Significantly lower rates of prescription of potent P2Y12 inhibitors were also noted for women, particularly for those with MVD. These findings warrant further investigation but suggest that both closer adherence to guideline-based therapy with respect to prescription of medication, and more complete revascularisation for those with MVD, may help to decrease sex-based outcome disparities for patients with STEMI.
Clinical Perspective
- This observational study found differences in treatment and outcome between men and women. Outcome differences persist after risk adjustment, driven primarily by differences in patients with multivessel disease (MVD) and/or with high residual SYNTAX scores.
- At early and late follow-up women with MVD experience cardiac death or MI at rates double those of men with MVD and all patients with single-vessel disease, and are significantly less likely to be prescribed guideline-directed potent P2Y12 inhibitors.
- A specific focus on improving adherence to guideline-directed prescription of medical therapy in women with MVD, along with more complete revascularisation for women with MVD may help to mitigate sex-based outcome disparities.