Vasoreactivity testing has received attention, as western cardiologists focus on the establishment of guidelines for patients with nonobstructive coronary artery disease (NOCAD).1 The prevalence of NOCAD determined at coronary angiography has been reported to be as high as 50%. Furthermore, two-thirds of patients with ischaemia and NOCAD have some sort of microvascular dysfunction.2,3 Despite the absence of obstructive coronary artery disease in these patients, they experience unfavourable clinical outcomes, including cardiovascular death and MI.
In the cardiac catheterisation laboratory, cardiologists are requested to perform rigid vasoreactivity testing when they diagnose patients with MI or ischaemia with NOCAD. These patients may experience coronary epicardial spasm (ES), coronary microvascular spasm (CMS) or coronary microvascular dysfunction (CMD).3 However, western cardiologists may prefer to evaluate CMD using a practice guidewire.4 They finally perform vasoreactivity testing to verify the presence of ES and CMS, even under the administration of nitroglycerin. In this article, we summarise the usefulness and clinical limitations of vasoreactivity testing and discuss future spasm provocation tests for use by cardiologists.
Intracoronary Acetylcholine Testing
Intracoronary acetylcholine (ACh) testing for patients with variant angina was first reported in 1986. The Japanese Circulation Society (JCS) guidelines recommended the original method proposed by Yasue and Okumura.5 We previously discussed the procedures, indications and exclusion criteria, and advantages and disadvantages of the ACh test in another review.6,7 We injected a maximum ACh dose of 80/200 µg into the right coronary artery/left coronary artery of patients in our study, in contrast to the JCS guidelines. The JCS guidelines recommend an intracoronary injection of ACh for 20–30 s with a pacemaker.
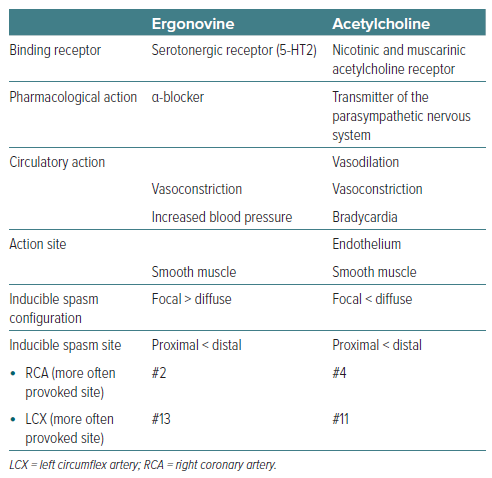
In contrast, the majority of western institutions, except for some special institutions, use intracoronary administration of ACh for 3 min without a pacemaker. We also reported that the administration time of ACh plays a key role in provoked spasms.8 Furthermore, we were able to perform intracoronary injection of maximum ACh 100 µg for 20 s into the left coronary artery without a pacemaker in more than half of the patients. The ACh testing method based on the JCS guidelines was developed for the documentation of coronary artery spasms, whereas the western ACh testing method was developed for the investigation of coronary endothelial dysfunction, not coronary spasms. The 3-min ACh administration is still not verified for the reproduction of coronary spasms in patients with vasospastic angina or variant angina. It is important for western cardiologists to verify the documentation of provoked spasm by 3-min ACh administration for patients with vasospastic angina.8 We showed the pharmacological characteristics of ACh (Table 2).
Intracoronary Ergonovine Testing
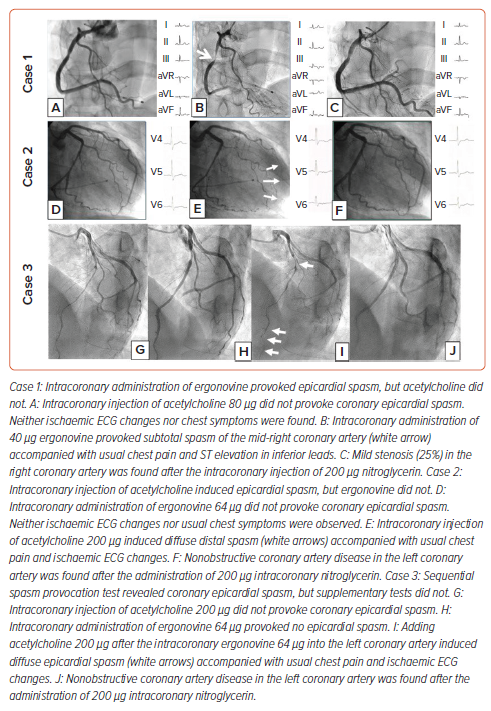
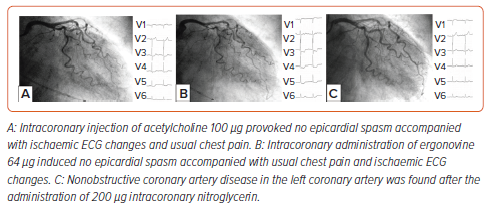
A few countries, including the US, Italy, France, Spain, Canada, South Korea and Japan, use the administration of ergonovine (ER) to verify the presence of ES and CMS. The majority of western cardiologists use intracoronary ACh testing instead of intracoronary ER testing. In another review, we reported the procedures, indications and exclusion criteria, and maximum ER dose.7 The JCS guidelines mention that the administration dose of ER is 20–60 µg in each coronary artery, although many cardiologists around the world use various doses of ER.5 An international standardisation of intracoronary ER testing should be constructed.7 ER acts through a serotonergic receptor. In our experience, some patients had ER-induced total spasms, but no spasms as a result of intracoronary ACh testing. We show a typical case in Figure 1 (case 1). We also show pharmacological characteristics of ER (Table 1).
Definition of Positive Spasm by Vasoreactivity Test
According to the Coronary Vasomotor Disorders International Study (COVADIS) Group definition of a positive ES, epicardial spasm (>90% vessel diameter), ischaemic ECG change and usual chest pain are necessary to diagnose a positive spasm.9 The JCS guidelines defined a positive spasm as >90% vessel diameter stenosis and ischaemic ECG change. However, the presence of all three issues is not always observed, even if patients had total or subtotal spasm according to vasoreactivity testing. Some researchers categorised an unclassified or unspecific group of patients who did not meet all three issues (epicardial spasm [>90% vessel diameter], ischaemic ECG change and usual chest pain). In the clinic, cardiologists should rightly use the term ‘suspected spasm’.
According to our previous reports, three-quarters of patients with >90% vessel diameter stenosis by intracoronary ACh testing, and two-thirds of patients with >90% vessel diameter stenosis by intracoronary ER testing meet all three criteria.10 However, the remaining one-quarter of patients with >90% vessel diameter stenosis by intracoronary ACh testing, and one-third of patients with >90% vessel diameter stenosis by intracoronary ER tests did not meet all three criteria.10
Single Spasm Provocation Test
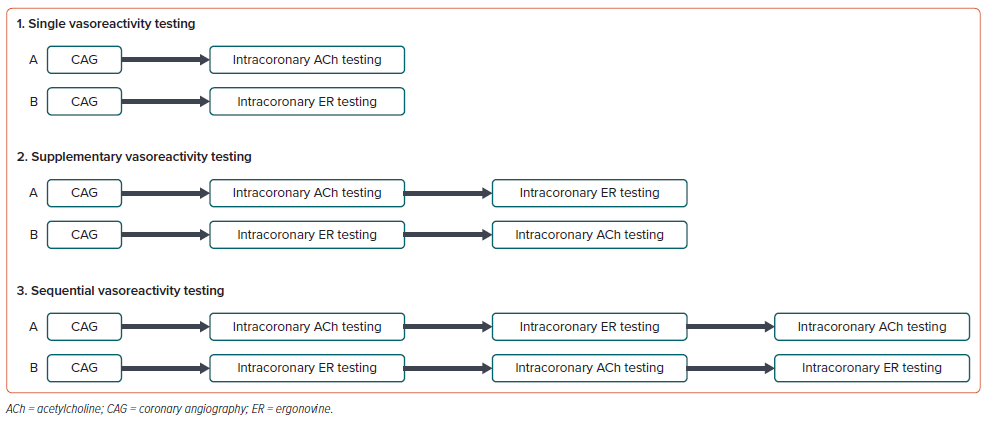
We experienced some cases of patients who had ACh-inducible spasm, but not ER, and vice versa.11 As shown in Figure 1 (case 2), intracoronary injection of ACh provoked typical spasms, but intracoronary administration of ER did not, while intracoronary injection of ER induced total spasms, but intracoronary injection of ACh did not, as shown in Figure 1 (case 1). Each pharmacological agent acts through a specific receptor, and cardiologists may obtain inducible spasm on one side when they perform single vasoreactivity testing (Figure 2). However, many cardiologists do not recognise this phenomenon because they use a single spasm provocation test to verify the presence of ES and CMS.
According to the analysis of previous vasoreactivity testing, we are the only institution in the world in which cardiologists perform both ACh and ER testing systematically in the same patients. We show the schema of the single, supplementary and sequential vasoreactivity testing in Figure 2. We added intracoronary ACh after the ER tests if a negative spasm had been induced by the ACh and ER tests. We did not perform the sequential vasoreactivity tests in Figure 2 (first intracoronary ER testing, second intracoronary ACh test and last intracoronary ER testing). General cardiologists should consider this method when diagnosing the presence of ES and CMS.
Supplementary Vasoreactivity Testing
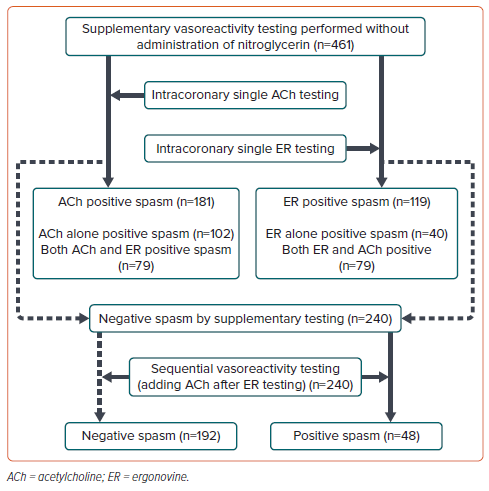
If cardiologists perform supplementary vasoreactivity testing to diagnose the presence of ES and CMS in all patients, some patients with ES and low disease activity may be missed. According to our previous report, as shown in Figure 3, ACh-inducible spasms, but not ER, were observed in 46% (102/221) of patients, whereas ER-inducible spasms, but not Ach, were revealed in 18% (40/221) of patients.12 Furthermore, both ACh- and ER-inducible spasms were recognised in 79 patients (36%) among 221 patients with ACh- or ER-inducible spasms. Each vasoreactivity test method (single or supplementary) has its own limitations related to inducing spasm. Cardiologists should understand the limitations of vasoreactivity testing in the cardiac catheterisation laboratory.
Sequential Vasoreactivity Testing
We have already reported the usefulness of sequential vasoreactivity testing in the clinic.12 We performed sequential vasoreactivity testing in patients with negative results for both tests, irrespective of strong suspicion of coronary artery spasm. We obtained a positive spasm in one-fifth of patients who had no spasm by intracoronary ACh and ER tests, as shown in Figure 3.
The clinical sensitivity (80%) and clinical specificity (78%) of the sequential vasoreactivity testing were low, but may be acceptable in the clinic. We recommend this sequential vasoreactivity testing in patients with low vasospastic angina disease activity, in those with resistant spasms and in survivors of coronary artery spasms treated with medications.13 A representative case (case 3) is shown in Figure 1.
Epicardial Spasm by Vasoreactivity Testing
In a large western cohort study of intracoronary ACh testing, ES was observed in 20% of patients with chest pain and NOCAD.14 Women were affected more frequently than men. Western studies used the 3-min administration of ACh, and they could perform these tests of the right coronary artery in just one-third of patients without a pacemaker.15 In contrast, Ohba et al. reported that ES was observed by intracoronary ACh testing in 216 (58%) out of 370 patients with angina and NOCAD.16 They performed testing of both coronary arteries in 91% of study patients. We recently reported that ES was revealed in 329 (44%) out of 746 patients with angina-like chest pain and NOCAD.17 In this study, we could perform vasoreactivity testing of both coronary arteries in 96% of study subjects. The incidence of ES in Japanese populations was markedly higher than that reported in studies of western populations.
Microvascular Spasm by Vasoreactivity Testing
CMD is frequently observed in western populations, especially in women. CMS was revealed in 33% (458/1,379) of patients with ischaemia and NOCAD in western studies.14 We could not determine the percentage of patients who underwent vasoreactivity testing of both coronary arteries in their study. Ohba et al. reported that CMS was diagnosed in 50 (14%) out of 370 Japanese patients with angina and NOCAD.16 We also reported that intracoronary injection of ACh revealed CMS in just 40 (5%) out of 746 Japanese patients with angina-like chest pain and NOCAD.17 Furthermore, ES coexisting with CMS or CMD was reported in a sizable proportion of patients. The frequency of CMS in Japanese subjects was significantly lower than that reported in studies of western subjects. We show a demonstrable case who had CMS on both ACh and ER testing in Figure 4.
Comparisons of Procedures and Populations Between Western and Japanese Studies
In western and Japanese studies, CMD is more frequently observed in women compared with men. However, the incidence of CMD in patients with ischaemia and NOCAD in western populations is remarkably higher than that in Japanese populations.18 This may be related to ethnic differences or diagnostic methodology variations. The intracoronary ACh administration time in western subjects is longer than that in Japanese subjects (180 seconds versus 20–30 seconds, respectively).19–21 According to our report, intracoronary administration time of ACh plays a key role in provoking positive spasms.8 If western and Japanese cardiologists performed the same vasoreactivity testing, including the same injection doses and the same injection time, we may learn the truth regarding ethnic differences. A prospective and randomised study is necessary to clarify the differences in epicardial and microvascular spasms among populations of different ethnicities.
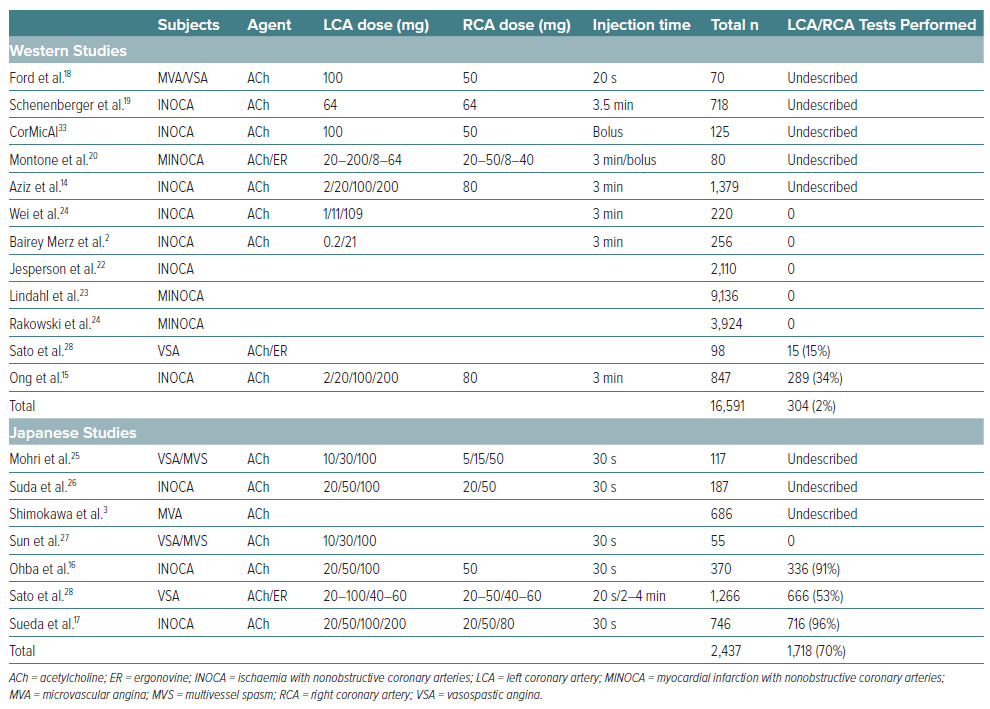
Necessity of Rigid Spasm Provocation Test When Cardiologists Diagnose Patients with Nonobstructive Coronary Artery Disease
In the previous reports shown in Table 2, we found the low frequency of both coronary vasoreactivity testing (median 11% [2,022/19,028; 0–96%]) when diagnosing patients with NOCAD. Furthermore, in some western reports, we could not find the vasoreactivity testing when they diagnosed these patients.22–24
Vasoreactivity testing should be performed in both coronary arteries to verify the presence of ES and CMS because ES and CMS are observed in both coronary arteries. In western studies, cardiologists focused on the evaluation of coronary vasomotor dysfunction in the left coronary artery.2,14,15,18 If they obtained no abnormal results, they performed vasoreactivity testing in the right coronary artery. This vasoreactivity testing performed by western cardiologists is sometimes insufficient for diagnosing ES and CMS. However, the vasoreactivity testing method used by Japanese cardiologists is still evolving, as shown in Table 2.25–28 Western and Japanese cardiologists should perform precise vasoreactivity testing when they diagnose the presence of ES and CMS in the cardiac catheterisation laboratory.
Complications of Vasoreactivity Testing
We previously reported complications during vasoreactivity testing in another review.29 In western studies, bradycardia was often observed due to the effect of ACh in patients without a pacemaker. In contrast, ventricular fibrillation or tachycardia necessary for electrical cardioversion is often found in Japanese reports.30 However, we could not find irreversible complications, including death, in recent reports. Buxton et al. reported three deaths due to severe spasm caused by performing intravenous ER tests.31 Selective vasoreactivity testing is a safe and useful method for patients worldwide.5,14 According to the COVADIS group and JCS guidelines, vasoreactivity testing was classified as a class I method.4,8
Future Vasoreactivity Testing
Cardiologists should understand the usefulness and limitations of single vasoreactivity testing for diagnosing the presence of ES and CMS. If we did not obtain positive results, we reported a negative vasoreactivity test, but we did not diagnose these patients with negative spasms. Cardiologists should reconsider a pseudonegative result when a negative vasoreactivity test is observed. If cardiologists strongly suspect ES and CMS, we recommend that they perform supplementary and sequential vasoreactivity testing to clarify the strict diagnosis, as shown in Figure 5.
Future vasoreactivity tests may involve a more complex technique. If western and Japanese cardiologists performed additional vasoreactivity testing to diagnose ES and CMS in the cardiac catheterisation laboratory, a more precise diagnosis of patients with NOCAD will be obtained in the future. Furthermore, guidewire-based evaluation of non-endothelial-dependent coronary microvascular function is recommended by the western reports and the European Society of Cardiology guidelines in patients with NOCAD.1,32,33 Non-invasive methods of CMD assessment, such as transthoracic echo Doppler, cardiovascular MRI or PET, are also useful for patients with NOCAD.
Conclusion
Vasoreactivity testing is essential for diagnosing patients with NOCAD. A single pharmacological spasm provocation test has limited efficacy for verifying the presence or absence of coronary ES and CMS. In the future, cardiologists should use supplementary or sequential vasoreactivity testing for patients with NOCAD, as needed.