Pulmonary hypertension is said to occur when the mean pulmonary artery pressure exceeds 25 mmHg at rest or 30 mmHg with exercise. The term pulmonary arterial hypertension (PAH) denotes a series of apparently unrelated disorders that share the histopathological entity known as plexogenic pulmonary arteriopathy (PPA).
There are many conditions that can lead to the development of pulmonary hypertension and these have traditionally been classified into five groups (World Conference on Pulmonary Hypertension, Venice 2003; Dana Point meeting on Pulmonary Hypertension 2008).
Those disorders listed in Group 1 share the histopathology of PPA although why such apparently diverse disorders should do so remains unclear. Examples of Group 1 disorders include idiopathic PAH, PAH associated with genetic factors (e.g bone morphogenetic protein receptor 2 mutations), connective tissue disorders (e.g systemic lupus erythematosis), portal hypertension, HIV and anorexigens, congenital heart diseases, pulmonary veno occlusive disease and pulmonary capillary haemangiosis. Advanced pulmonary vasodilator therapy is given to patients who have pulmonary hypertension associated with these conditions.
Group 2 disorders comprise left heart disorders e.g valvular disease and atrial or ventricular dysfunction while Group 3 diseases reflect pulmonary hypertension in association with lung disease or hypoxemia e.g chronic obstructive pulmonary disease (COPD), interstitial lung disease or sleep disordered breathing.
Pulmonary hypertension associated with chronic pulmonary thremboembolism is included in Group 4 and Group 5 and comprises miscellaneous conditions with unclear or multifactorial aetiologies such as histiocytosis, lymphangioleiomyomatosis, glycogen storage disease, Gaucher disease and post splenectomy.
Pathology
It is possible that the lung has only a small number of responses to injury that feed into common final pathway mechanisms. Many insults can lead to the development of the acute respiratory distress syndrome (ARDS) but the pathology is similar (and not PPA) regardless of initiating injury. Similarly obliterative bronchiolitis seen as a consequence of rheumatoid arthritis or infection with respiratory syncytial virus in children is similar to that believed to be a form of chronic allograft rejection in lung transplant recipients.
In PPA there is an initial period of vasoconstriction followed by migration of smooth muscle cells from the inner half of the media of muscular pulmonary arterioles into the lumen. Here they become myofibroblasts that are capable of laying down both smooth muscle and fibrous tissue. The myofibroblasts proliferate in a concentric fashion and, upon sectioning, the vessels look like a cut onion, hence the term ‘onion skin proliferation’. This leads to a progressive reduction in the radial size of the vessel, the resistance to flow increases in accordance with Poiseuilles law (where among other things flow is proportional to the fourth power of the radius, r4) vessel rupture at proximal points of weakness (e.g. at branches) occurs. Haemorrhage ensues and primitive networks of blood vessels (a ‘plexus’, hence plexiform lesion) grow into the area. The combination of onion skin (or concentric laminar intimal) proliferation and plexiform lesions is known as PPA.
It is possible that patients may have a genetic predisposition or risk factor, such as a connective tissue disease or HIV, and that this causes a vascular injury or modification in antigenic determinants. Endothelial cell dysfunction follows with derangement of the normal release of endothelial derived factors, which facilitates inflammation and promotes loss of local vaso reactivity and thrombus formation. Decreased progression and vascular remodelling can then occur. The pulmonary endocrine cells immuno reactive for calcitonin and gastrin releasing peptide may adversely influence smooth muscle cells.
Diagnosis
Although there is increasing awareness among clinicians regarding pulmonary hypertension, much more work needs to be carried out to promote earlier and accurate diagnosis. The clinical features are often non-descript and include fatigue, malaise, chest pain, palpitations, pre-syncope or syncope or haemoptysis. Additionally, the diagnosis may not be considered in patients with co-existing cardiac or pulmonary disease and yet underlying pulmonary hypertension may be the reason for the apparent failure to respond to conventional treatment of their primary disease. Furthermore, it is essential that pulmonary hypertension is carefully assessed and optimised where appropriate if patients are required to undergo intervention (e.g surgery) or should they become pregnant. In addition to history and clinical examination the following investigations are routinely performed to assess patients with suspected pulmonary hypertension;
- Routine haematological and biochemical parameters including autoimmune profile, HIV serology and thrombophilia screen (if pulmonary embolism is suspected) or genetic studies if familial PAH is being considered and BNP.
- Chest X-ray.
- Electrocardopgram (ECG).
- 2D echocardiography.
- Lung function tests and arterial blood gas analysis.
- Thoracic computed tomography (CT) scan/CT pulmonary angiography or ventilation–perfusion (VQ) scan.
- Right heart catheter.
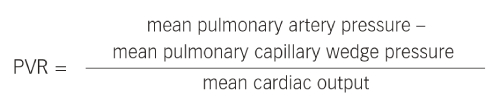
This investigation is considered gold standard for diagnosing patients with pulmonary hypertension and provides information regarding right arterial pressure, pulmonary arterial pressure, right ventricular pressure, cardiac output and mixed venous (pulmonary arterial) oxygen saturation and left atrial filling pressure (the pulmonary capillary wedge pressure). The pulmonary vascular resistance (PVR) is derived from the formula:
The PVR can be indexed (PVRi) and the systemic vascular resistance can also be calculated and indexed (SVRi).
Other tests that may be performed include exercise test, magnetic resonance imaging (MRI), overnight oximetry and, occasionally, pulmonary angiogram.
Disease Progression
At onset there may be few symptoms, but as the disease progresses the PVR rises and the cardiac output falls. Common symptoms include dyspnoea on exertion or at rest, chest pain (due to right ventricular angina), palpitations and pre-syncope or syncope. Ultimately the signs and symptoms of right heart failure develop and death occurs. A median survival of 2.8 years has been reported for untreated patients in New York Heart Association (NYHA) class III or IV. Sudden acute elevations in PVR can occur (known as pulmonary hypertensive crises) leading to an acute reduction in left heart filling and profound systemic hypotension and can sometimes be fatal. This can occur during general anaesthetic induction and is one of the reasons why patients with PAH need careful preoperative evaluation prior to surgical intervention.
Treatment
In general, if pulmonary hypertension occurs in association with other conditions, treatment of the primary disorder should be optimised first. Algorithms for the treatment of PAH vary around the world. Typically therapeutic agents specifically targeting pulmonary hypertension are given to those patients who are in Groups 1 and 4 and these who are in renal failure on dialysis. Advanced pulmonary vasodilation therapy is prescribed if the mean pulmonary artery pressure exceeds 25 mmHg and the mean pulmonary capillary wedge pressure is <15 mmHg. Such therapy is usually given to patients who are in World Health Organization (WHO) functional class II, III or IV.
There is concern that treating patients with pulmonary vasodilating agents whose left atrial filling pressure exceeds 15 mmHg will lead to increased venous return to the heart that in turn could lead to, or exacerbate, left heart failure.
There is little evidence to justify treating patients with advanced pulmonary vasodilator therapy who have pulmonary hypertension associated with lung disease. Those with obstructive sleep apnoea should have appropriate treatment e.g with nocturnal nasal continuous positive airway pressure (CPAP) and lifestyle advice and only have consideration given to treating pulmonary hypertension should it persist after standard therapies for sleep disordered breathing having been tried.
There is no effective cure for patients who develop PAH but specific targeted therapeutic agents have been shown to improve exercise capacity, WHO functional class, haemodynamic parameters and time to clinical worsening. Recently there has been a suggestion that a newer endothelin receptor antagonist (ERA) may be associated with improved survival although further studies are needed to confirm this. However, it is accepted that the prognosis for patients with PAH is improving.
Approximately 10 % of patients with PAH will respond to calcium channel blockers, and such patients will usually demonstrate reversibility (a reduction in mean pulmonary artery pressure by >10 mmHg to achieve an absolute value of <40 mmHg with an unchanged or increased cardiac output) at right heart catheterisation.
Sildenafil and tadalalfil are phosphodiesterase 5 inhibitors and act on the nitric oxide pathway to cause vasodilation. Sildenafil may also possess anti proliferative effects on vascular smooth muscle. A newer class of agents, soluble guanylate cyclase stimulators, reduce intracellular calcium in an NO dependant and independent fashion and have been used to treat patients with PAH and chronic thromboembolic pulmonary hypertension (CTEPH).
Endothelin levels are increased in PAH and relate to disease severity and prognosis. Different ERA can block one (A) or both of the endothelin receptors (A and B) to antagonise vasoconstriction and vascular remodelling promoted by excessive endothelin release.
The deficiency of endogenous prostacyclin can be addressed by administration of prostacyclin or its analogues by continuous intravenous (IV) infusion, by regular inhalational therapy or by subcutaneous injection. The precise role of combination therapies and the timing of their introduction into the therapeutic regime of the PAH patient is being evaluated. Other therapies under trial include lipid- lowering drugs, anti-inflammatory agents, monoclonal antibodies and anti-platelet agents.
Atrial septostomy is available for a small number of patients with class IV disease in an attempt to offload the failing right ventricle as a bridge to transplantation.
Thereisencouragingexperiencewithpulmonarythromboendarterectomy for selected patients with CTEPH. However, this is a major operation with a high (almost 50 %) complication rate. Bilateral lung transplantation is available for some patients with PAH but donor organ availability and the late complication of obliterative bronchiolitis remain major problems to be addressed.
Conclusion
PAH is a progressive and lethal disease whose initial symptoms are non-specific. Improved awareness is required to enable patients with PAH to be diagnosed earlier and to have their disease carefully characterised and receive appropriate therapeutic intervention as soon as possible. Patients with PAH should be managed in a centre with specialist clinicians and nurses who are trained in the assessment and management of these challenging patients (often in conjunction with a local hospital) and who are available to offer advice and support when complications arise, should patients become pregnant or should surgical intervention be necessary.
It is hoped that an improved understanding of the pathophysiological mechanisms involved in PAH will lead to the development of more effective treatments.