Heart Failure – A Major Global Health Problem
Cardiovascular diseases (CVDs) remain the leading cause of morbidity and mortality in developed countries and its burden is progressively increasing.1–4 Coronary artery disease (CAD) and other conditions, such as hypertensive heart disease or diabetes mellitus, are rated among the foremost reasons for morbi-mortality worldwide.1–4 In this context, heart failure (HF) has emerged as an extremely important condition that appears to be reaching epidemic proportions. The reported prevalence and incidence of HF varies depending on the studies considered, the definitions used, subjects included in studies and quality of data recorded.5,6 An overall prevalence of 1–2 % has generally been reported in western countries,5–7 and this is considerably higher in the elderly i.e. >10 %.6,8 From the Framingham Heart Study it has been estimated that in the general population the lifetime risk of developing HF at the age of 40 is as high as 20–21 %,9 and these figures were reported by the Chicago Heart Association Detection Project in Industry (CHA) and the Cardiovascular Health Study (CHS)10 to be even higher (20 % to 42 % at age 45, depending on gender and race). Progressively better and more-effective management of HF in the last decades has improved patient survival but its incidence has remained stable;5,7 hence the burden imposed by HF, as a chronic disease, on both health systems and the individual, has increased, affecting mainly the elderly.5–7 Despite a reduction in hospitalisation and mortality rates in the past years, these remain high.5–7,11 Indeed, age- and sex-standardised hospitalisation rates of 468 and 1,359 per 100,000 people for primary and secondary HF, respectively, have been reported in the US in 2009.11 Moreover, in the population-based Rotterdam Study, survival rates after incident HF in subjects ≥55 years old were 86 %, 63 %, 51 % and 35 % at 30 days and 1, 2 and 5 years of follow-up, respectively.8 These data underscore the importance of HF as a major global health problem and the need for having reliable and accurate tools that facilitate decisions regarding its prevention, management and outcomes. In this context, the interest in identifying novel biomarkers that can aid diagnosis, risk stratification, prognosis and treatment strategies, has grown considerably in recent years.
Biomarkers in Heart Failure
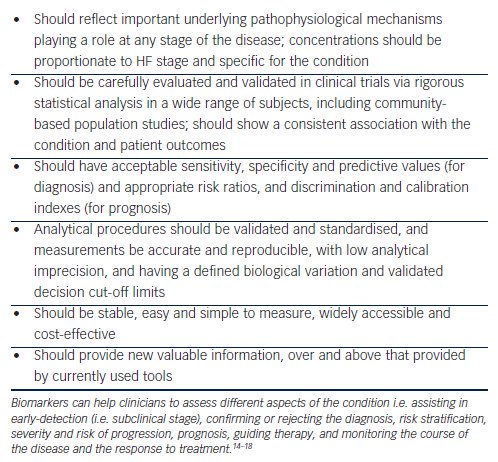
HF is primarily diagnosed in the presence of symptoms and signs that, in many cases, are non-specific.7,12 Symptoms of HF result from an impairment in the normal heart function as a consequence of structural or functional disorders affecting ventricular filling and/or blood ejection.7,12 Recently, biomarkers such as brain natriuretic peptide (BNP) or amino-terminal pro-brain natriuretic peptide (NT-proBNP) have emerged, which appear to represent an important tool for diagnosis, risk stratification and prognosis.7,12 A biomarker has been defined as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention”.13 Although this definition is wide and can include any measured parameter, the term ‘biomarker’ is more commonly used in relation to biological substances that are detected in body fluids. Figure 1 summarises the characteristics that make a biomarker useful in clinical practice in the context of CVD and HF.14–18
Natriuretic Peptides
Based on the results of studies such as the Breathing Not Properly Multinational Study,19 ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE),20,21 Rapid Emergency Department Heart failure Outpatient Trial (REDHOT),22 Valsartan Heart Failure Trial (Val-HeFT),23 Groenning et al.24 or the International Collaborative of NT-proBNP Study,25 among others, international guidelines on both acute and chronic HF (AHF/CHF) describe a role for BNP and NT-proBNP in the diagnosis and prognostic assessment of HF.7,12,15,26–29 Additionally, increasing evidence is emerging about a possible role for natriuretic peptides (NP) to guide therapy.12,30 However, despite their usefulness and increasing use in clinical practice, some limitations must still be acknowledged. For instance, the optimal cut-off points are still not well-established and different thresholds have been proposed;18,27,31–33 additionally, there is a range of values (a ‘grey zone’) where they are less helpful in decision-making;27,31,32 furthermore, while low NP concentrations make the diagnosis of HF unlikely (high negative predictive value), increased levels can be also a consequence of several cardiac and non-cardiac conditions.7,12,27 Levels of NP can also be affected by factors such as age, obesity, anaemia and renal function.12 In addition, NP are released as a result of myocyte stress caused by pressure or volume overload;16,34,35 therefore, they may not completely reflect other mechanisms within the complex pathophysiology of HF (e.g. renin–angiotensin–aldosteron system; autonomic nervous sytem). Finally, more evidence is needed in relation to the use of NP to guide therapy. This aspect has been approached in different trials comparing a strategy based on BNP or NT-proBNP-guided therapy versus the usual or standard care;36 however, many of these studies were small, lacked power to assess major end-points and their results were not always consistent.12,30,36 More recently, several meta-analyses have suggested that NP-guided therapy strategies could be associated with a reduction in all-cause mortality and HF-related hospitalisations in CHF;30,36–42 this is of interest, but the findings seemed to be influenced by age as it was mainly observed in individuals aged <70–75 years.30,36,39–42
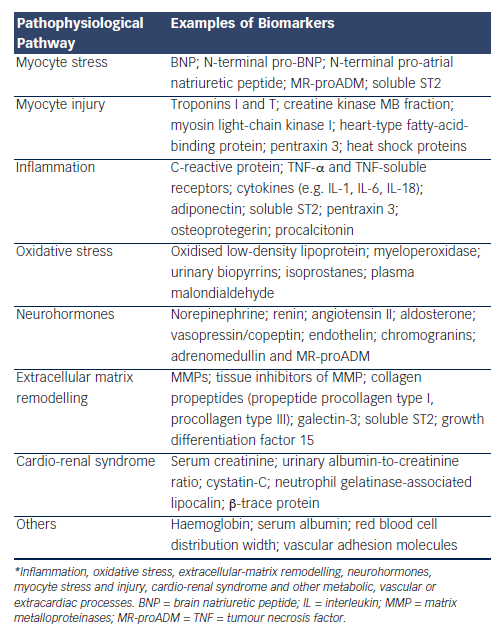
Better understanding of the role of NPs in clinical practice and their contribution to the diagnosis and management of HF in recent years16,18 has stimulated research into newer biomarkers. As an example, Table 1 shows a classification of established and novel biomarkers.15,16,34,35 A multi-marker strategy, covering different and complementary aspects of HF in an integrated algorithm, has been proposed and may improve both diagnostic and prognostic assessment strategies.43–45 The incorporation of newer biomarkers may however potentially increase the complexity of the assessment and costs, a matter that will need to be explored in due course.
Soluble ST2 – An Emerging Biomarker
The interleukin-1 receptor-like 1 (IL1RL1) protein, commonly referred to as ST2 (growth stimulation expressed gene 2), has emerged as a promising novel biomarker for AHF and CHF46–49 and other related conditions, such as CAD50,51 and hypertension.52 While soluble ST2 (sST2) lacks disease specificity, which may limit its role in the diagnosis of HF,53 it may have a role regarding prognosis assessment in HF. The recent American College of Cardiology/American Heart Association (ACC/AHA) guidelines on HF management state that ST2 can provide additive value regarding risk stratification, particularly in patients with acutely decompensated HF (Class IIb, level of evidence A) and those with CHF (Class IIb, level of evidence B).12 sST2 was first described in 1989 by Klemenz et al.54,55 and Tominaga.56 It was independently identified and subsequently designated as T1,54,55 ST,2,56,57 delayed early response gene 4 (DER-4)58 and Fit-1 (the homologue of mouse ST2/T1 protein).59 The expression of the IL1RL1 gene generates three different messenger RNA (mRNA) isoforms by alternative 3’ splicing: a membrane-bound (ST2L), a secreted (sST2) and a variant (ST2V) protein.57,59–63 ST2L is a transmembrane receptor expressed in the cell surface, having an intracellular domain, a single transmembrane domain and an extracellular domain formed by three immunoglobulin (Ig)- like repeats.57,59,61,64 Like the rest of the members of the IL-1 receptor/tolllike receptor (IL-1R/TLR) superfamily, it has a cytosolic toll/IL-1 receptor (TIR) domain responsible for signalling after receptor activation;64–66 and as part of the type I IL-1 receptor (IL-1RI)-like subfamily, it has extracellular Ig-like domains responsible for ligand binding.64 The sST2 form can be measured in circulating blood and consists of the extracellular domain only, lacking the transmembrane and intracellular ones; it is considered to act as a decoy receptor, competitively binding IL-33, hence preventing its effect through the ST2L receptor.57,59,61,67–70 The third ST2 form (ST2V) is the result of an inserted nucleotide sequence in the middle of ST2 DNA, leading to the absence of the third Ig-like domain;62 it seemed to have a different expression pattern from sST2 and ST2L,63 and the importance and physiological role of this variant remain unknown.
ST2 and Functional Ligands — Interleukin-33 and IL-33/ST2 Signalling
Despite that ST2 was first described in 1989, it was not until 2005 when the IL-33 was identified as its functional ligand.71 Secreted IL-33 mediates its effects in target cells by binding ST2L,66,71,72 as part of the IL-33 receptor (IL-33R) complex; this is a heterodimeric receptor constituted by the ST2L transmembrane protein, which is the ligand-binding subunit, and by the so-called IL-1 receptor accessory protein (IL-1RAcP), which seems to be necessary for the IL-33-mediated signal transduction and its effects in vivo.66,72,73 Once IL-33 binds the IL-33R complex, signalling is induced through the TIR domain, leading to the recruitment of different proteins (e.g. myeloid differentiation primary-response protein 88 [MyD88], IL-1R-associated kinases [IRAK], tumour necrosis factor [TNF] receptorassociated factor 6 [TRAF-6]) and subsequent activation of different signalling pathways (e.g., transcription nuclear factor-κB [NF-κB] pathway, mitogen-activated protein kinases [MAPK] pathway, PI3K/Akt), which ultimately leads to the production and secretion of different inflammatory factors, chemokines and cytokines.67,70,71,73–81
IL-33 is widely expressed in many tissues, including the heart,71,74 and in many cells, including, among others, endothelial and smooth muscle cells, cardiomyocytes, fibroblasts or macrophages.71,74,78,82 A dual role for IL-33 has been described, both as a cytokine released from the cells (cytokine-like, therefore binding ST2L in target cells), and as an intracellular nuclear factor (nuclear factor-like).74,75,79,83 In fact, IL-33 was first described as a nuclear factor with a DNA-binding domain present in endothelial cells.84 A nuclear location of IL-33 has later further confirmed, although the pathophysiological role of IL-33 as a nuclear factor is not well-known;78,82,85–88 different studies have suggested that IL-33 could play a role as a danger endogenous signal, which would be released as an active full-length protein to alert cells of immune system during damage or infection, whereas in case of apoptosis IL-33 would be cleaved and inactivated by caspases, preventing an inflammatory response in case of programmed cell death.74,75,78,79,82,83,89–93 This would be supported by the wide expression of IL-33 in cell types in normal human tissues,71,74,78,79,82,88,89 suggested to be constitutively expressed in the nucleus of several cell types, including human endothelial cells, fibroblasts, cardiomyocytes and coronary artery smooth muscle cells.78,82,88
Soluble ST2 in the Cardiovascular System
The expression of ST2 in the cardiovascular system was first described by Weinberg et al. in 2002, when the authors observed that serum levels of ST2 and levels of mRNA ST2 in left ventricular (LV) tissue were significantly increased in rat cardiomyocytes subjected to mechanical strain and in an in vivo model of experimental myocardial infarction (MI) in mice by ligation of a coronary artery compared with controls not subjected to these procedures.94 These experimental results were also supported in humans after studying 69 patients with acute MI randomly selected from the Healing and Early Afterload Reducing Therapy (HEART) study: serum ST2 levels at day 1 were significantly higher compared with those at days 14 and 90, and correlation studies suggested that ST2 might be related with the extent of myocardial injury or biomechanical load after MI.94 Later studies have confirmed and expanded these initial findings, demonstrating a cardioprotective effect of IL-33 through ST2 signalling, in both in vitro and in vivo models.67,68,71,76,78,80,86,95 For instance, treatment with IL-33 was found to reduce the infarct volume and fibrosis in rats 15 days after ischaemia-reperfusion injury, as well as to improve echocardiographic and invasive haemodynamic parameters, suggesting that the beneficial structural changes produced by IL-33 may also lead to a better cardiac contractile function.68 Sanada et al. confirmed a role of IL-33/ST2 signalling in controlling cardiomyocyte hypertrophy and cardiac fibrosis in vitro (rat neonatal cardiomyocytes and cardiac fibroblasts subjected to biomechanical strain) and in vivo (pressure overload induced by transverse aortic constriction [TAC]);67 additionally, administration of sST2 decreased the antihypertrophic effect of IL-33 in a dose-dependent manner, and blocking the ST2L receptor with an anti-ST2L monoclonal antibody also eliminated the effects of IL-33, unlike controls.67 These results have been further confirmed in vivo in ST2-null mice, lacking both ST2L and sST2 (ST2-/-) subjected to TAC;67,68 compared with wild-type mice, ST2-null mice showed increased cardiac fibrosis and hypertrophy, macrophage infiltration, impaired echocardiographic parameters (including impaired systolic function or increased left ventricle dilation), increased gene expression of NP or increased mortality; by treating with IL-33, these findings were reduced and survival improved in wild-type mice but not in ST2-/-.67,68 Different mechanisms, such as inhibition of cardiomyocyte apoptosis and increased expression of anti-apoptotic proteins, reduced mast cell density in infarct areas, promotion of a shift towards a Th2 response in lymphocytes, involvement of cardiac stem cells influencing processes as regeneration, differentiation or repairing after injury (autocrine or paracrine signalling), inhibition of cardiac fibroblasts migration or activation of different cytokines expression, among others, have been suggested to be involved in the beneficial effects of the IL-33/ST2 pathway.68,76,78,95
Altogether, data from both in vitro and in vivo models suggest a cardioprotective effect of IL-33 through ST2 signalling: IL-33, mechanically or by injury (ischaemia) induced in both, cardiac fibroblast and cardiomyocytes, and acting as a ligand for the ST2L receptor, would play a favourable cardioprotective role against hypertrophic-, fibrotic- and inflammatory-related signals following mechanical overload or injury; sST2 would act as a decoy receptor that binding IL-33 in blood prevents its action through the ST2L receptor.
An atheroprotective role of IL-33 through ST2L signalling, counteracted by sST2, has also been described,69,70,81,96,97 including a reduction in the atherosclerotic lesion size,69 lower macrophage foam cell accumulation in the plaques97 or promotion of angiogenesis.81 A modulatory role of IL-33/ ST2L in the inflammation of atherosclerosis has been proposed to explain these effects, such as promoting a Th1-to-Th2 switch response (Th2- mediated immunity),69 increased levels of oxidised-low-density lipoprotein (LDL) antibodies,69 regulation of adhesion molecules70 or an increased activity of T-reg cells.96
Soluble ST2 and Prognosis in Chronic and Acute Heart Failure
Soon after its relation to the CV system was described, sST2 was suggested to be associated with prognosis in CHF; in 161 patients with severe CHF (New York Heart Association (NYHA) III-IV, LV ejection fraction [LVEF] <30 %) from the Prospective Randomized Amlodipine Survival Evaluation 2 (PRAISE-2) study, Weinberg et al. found sST2 changes from baseline to 2 weeks to be significantly associated with mortality or heart transplantation, independent of BNP or proANP;98 in this first study, however, baseline sST2 was not significantly associated with events, unlike BNP.98 Later studies with larger cohorts and longer follow-up, including analyses from the Penn HF Study, CORONA (Controlled Rosuvastatin Multinational Trial in Heart Failure), HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training), PROTECT (ProBNP Outpatient Tailored Chronic Heart Failure) or Val-HeFT studies, among others, have supported higher baseline sST2 to be a predictor of adverse outcomes, such as all-cause, CV or HF death, sudden cardiac death or hospitalisation.46,47,99–102 In these prognostic studies, sST2 levels have been found to be higher in subjects with more advanced disease, such as increased NYHA class, higher NTproBNP or worse renal function;46,101 some studies also suggest its levels to be higher in males,46,99,101 though the effect of gender as well as other factors such as the ethnicity or HF aetiology are not well established. However, the prognostic value of sST2 in CHF seems not to be significantly influenced by renal function.103 The role of sST2 compared with NP remains more controversial. In many of the studies, sST2 was reported to be a significant predictor of adverse events in multivariable adjusted models including NP and it improved risk stratification;46,100–102,104 however, in the CORONA study this relationship was no longer significant after including NTproBNP (together with C-reactive protein) in the models (except for the secondary outcomes of HF death or CV or HF hospitalisation).47 In analyses from Val-HeFT, when NTproBNP was included in the models, sST2 did not add significant prognostic information.99 And in HF-ACTION, sST2 did not improve significantly reclassification of risk in models already containing NTproBNP.101 Most of the prognostic studies in CHF have been focused mainly in patients with systolic HF, with low LVEF (mean/median around 30 %), so its value in HF with preserved LVEF is uncertain; finally, many of them are post hoc analysis or sub-studies from previous larger trials not specifically designed to assess sST2.
Apart from CHF, sST2 has been reported to be consistently associated with prognosis in AHF as well as in patients attending the emergency department (ED) with dyspnoea. In a large cohort of over 1,000 subjects presenting with dyspnoea at ED, Socrates et al. found higher sST2 to be predictive of mortality at 1 year even when including NP in multivariable adjusted models (in both all participants with dyspnoea and in those with AHF as the cause for such symptoms).48 This association with mortality was consistently confirmed in other studies;49,105–107 also with in-hospital mortality;108 and in the PRIDE study the predictive value remained significant at a longer follow-up of 4 years.109 In these reports, the baseline levels of sST2 have been repeatedly found to be higher in those patients with AHF as the cause of dyspnoea and among decedents during the follow-up than in survivors.48,49,106,108 Likewise, results suggest that its levels are lower in HF with preserve LVEF compared with systolic HF,48,107 though it remained an independent predictor of mortality in both situations.107 Changes in the decompensated status of patients following management and therapy of AHF could have its reflection in the levels of biomarkers. In this respect, serial measurements of sST2 from presentation to a variable time (e.g. first 48 hours,108 admission to discharge110 or baseline to 2 weeks111) have been reported. In these studies, a failure of sST2 levels to decrease from baseline (a certain percentage reduction, again variable depending on the study) has been associated with subsequent mortality108,110 or cardiac events111 in the following months. These observed dynamic changes of sST2 according to the clinical status and response to HF management may suggest a potential role of this biomarker for monitoring the course of the disease and response to therapy,53,111 though this aspect needs to be specifically studied and confirmed.
Summary and Conclusions
In the HF context, some biomarkers constitute a valuable tool that can help physicians address more efficiently the management of the different stages of the disease, from early detection and diagnosis to risk prediction and also guiding therapy. While many biomarkers have been studied over the last years, only a few of them have been accepted for use in clinical practice. Nowadays, B-type-related NP are probably the most established biomarkers in clinical practice for both AHF and CHF diagnosis and management. Specific recommendations about their use have been released in international guidelines. However, limitations of these biomarkers for the management of HF do exist and therefore the search for newer biomarkers continues unabated. Some of the novel emerging biomarkers may provide useful additional information over and above that of currently used markers. This may be the case for sST2, for which increasing evidence points toward its utility as a prognostic marker in AHF and CHF. However, more work and studies specifically designed to assess its value in HF are required before ST2 can be incorporated to everyday clinical practice







