Atrial fibrillation (AF) is the most common clinically significant arrhythmia, which confers a substantial morbidity and mortality from stroke, thromboembolism and heart failure.1−4 Gender-related differences in the presentation, treatment and outcome of patients with AF have been previously reported. Female patients with AF tend to be older and more frequently have hypertension, heart-valve disease and thyroid dysfunction,4−14 while male patients with AF are more likely to be smokers or to have ischaemic heart disease and abnormal left ventricular ejection fraction (LVEF).4,6−13
Compared with male AF patients, females with AF are more symptomatic,6,9,12,14 and are more likely to be treated with calcium channel blockers13,14 or diuretics.5,8,13 In addition, women are less frequently treated with amiodarone8,11,14 and undergo electric cardioversion.11,14 Moreover, the risk of stroke7,10−12 and of adverse events following administration of antiarrhythmics, statins or anticoagulants6,10,12 is increased in females.
Increased mortality in women versus men with AF has been reported in a number of studies.4,5,7 By contrast, other investigations found no significant sex-related differences in mortality in AF patients.8,9,11,14 Moreover, information regarding the impact of clinical variables on survival of females compared to males with AF is scarce. In the RAte Control versus Electrical cardioversion for persistent atrial fibrillation (RACE) study females but not males with recurrent persistent AF demonstrated enhanced cardiovascular morbidity and mortality under the rhythm control approach, as compared to the rate control approach.9 Hypertension, coronary artery disease and valve disease were associated with poor prognosis only in men.9 It is conceivable that additional clinical variables, not yet evaluated, might have a different impact on the survival in men versus women.
Gender-related differences have been studied in a variety of patient populations with AF, including outpatients,4,5,7,11,14 patients with a non-valvular,10 new-onset6,14 or permanent13 AF, and patients participating in drug-oriented trials.8−10 AF is a common reason for admission to an internal medicine ward and may also appear during hospitalisation for various disorders other than AF. Surprisingly, limited data are available concerning the gender-related differences in the clinical characteristics and prognosis of this patient population. We aimed to prospectively evaluate various clinical variables and their association with long-term survival in females versus males hospitalised in an internal medicine ward with paroxysmal/persistent AF.
Methods
Study Design
The study population included 250 adult patients randomly admitted from the Emergency Department to our department (one of the six Departments of Internal Medicine, in our Medical Centre) for a variety of medical disorders. These patients either had paroxysmal or persistent AF on admission or developed AF during hospitalisation. Patients with unknown AF duration and permanent AF were excluded. Informed consent was obtained from each patient. The study was carried out in accordance with the Declaration of Helsinki and was approved by the local Ethics Committee.
Data Collection
Demographic, clinical, electrocardiographic (ECG), echocardiographic and laboratory data of the patients were collected following admission. On discharge, the following additional data were registered:
- presence of recurrent episodes of AF during hospitalisation;
- time from the AF onset to conversion to sinus rhythm;
- ECG rhythm;
- duration of hospital stay; and
- recommended medications.
Following discharge, all-cause mortality was recorded and death was confirmed by hospital or outpatient death certificates. At the end of the follow-up period extending up to five years, the data were subjected to statistical analysis.
Definitions
Anaemia, according to the WHO criteria, was defined as a haemoglobin concentration of <13 g/dl in men and <12 g/dl in women. Renal function was assessed by estimating the glomerular filtration rate (GFR) using the Modification of Diet in Renal Disease (MDRD) equation.15 Renal dysfunction was defined as GFR <60 ml/min/1.73 m2. Valvular disorder was defined as a moderate or severe insufficiency and/or stenosis of any cardiac valve.
Statistical Analysis
By comparing the data obtained for the male and female groups statistical evaluation was performed. Pearson's chi-square or Fisher’s exact test, as appropriate, was used for comparison of qualitative variables. Two-way analysis of variance (ANOVA) was adopted for quantitative variables. To determine the prognostic significance of the variables, survival curves were plotted using the Kaplan–Meier estimate. Mantel–Cox and Breslow tests were applied to evaluate the differences between the curves. Variables significantly associated with survival when assessed by the Kaplan–Meier method (p≤0.1) were re-evaluated by the Cox proportional-hazards model, to identify the variables most significantly associated with mortality. A p-value ≤0.05 was considered statistically significant. The data were analysed using BMDP Statistical Software.16
Results
Characteristics of the Patients
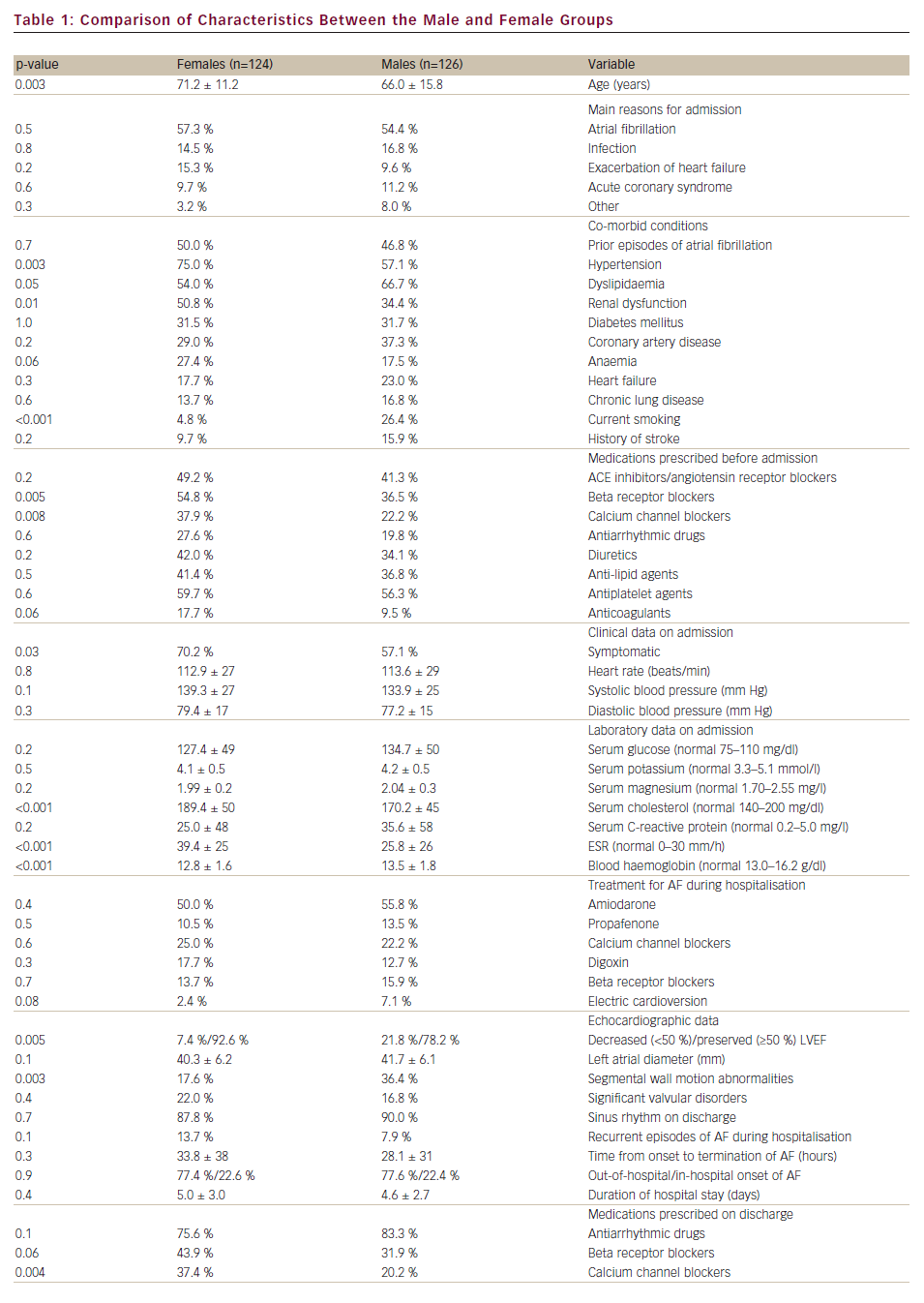
Table 1 presents the comparison of demographic, clinical, laboratory and echocardiographic data between the male (126 patients) and female (124 patients) groups. The women were significantly older than men (p=0.003).
No significant differences in the reasons for admission between the groups were recorded (see Table 1). Hypertension (p=0.003) and renal dysfunction (p=0.01) were found more common in women. Dyslipidemia (p=0.005) and smoking (p<0.001) were more frequent in the men. Before admission, females were more likely to be treated with beta receptor or calcium channel blockers (p=0.005 and 0.008, respectively). On admission, women were more symptomatic than men (p=0.03), while mean values of heart rate and blood pressure were comparable between the groups.
Significant gender-related differences were also observed in laboratory data. Women had higher mean levels of cholesterol and erythrocyte sedimentation rates (ESR) as well as lower haemoglobin (p<0.001 for all comparisons). On echocardiographic examination, the proportion of patients with decreased LVEF and with segmental wall motion abnormalities (p=0.005 and 0.003, respectively) was significantly higher in males.
Treatments provided for AF during hospitalisation were not significantly different between the groups. Similarly, no significant differences were observed with respect to the rates of conversion of AF to sinus rhythm, presence of recurrent episodes of AF during hospitalisation, meantime elapsing from the onset to the termination of AF, duration of hospital stay and proportions of patients with out-of-hospital versus in-hospital onset of AF. Women were more frequently discharged with prescriptions of calcium channel blockers (p=0.004) or diuretics (p=0.009).
Survival
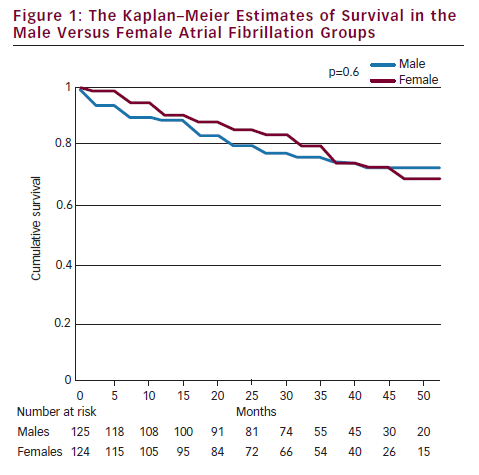
Follow-up (median period of 39-months) was completed in 249 patients, since one male patient dropped out of the follow-up. Figure 1 shows survival curves in males versus females. Survival rates, as well as mean survival durations, were not significantly different between men and women (78.4 versus 79.0 % and 45.7 versus 45.5 months, respectively, p=0.6).
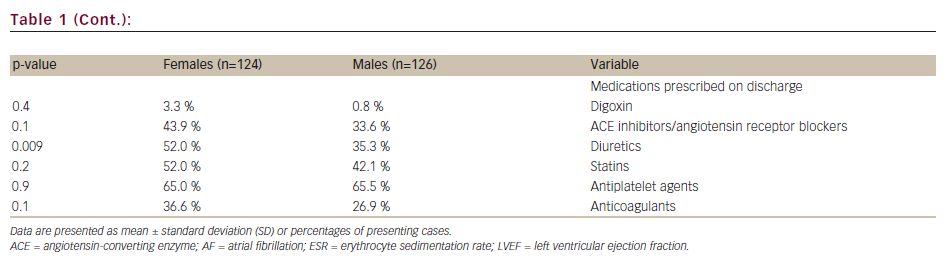
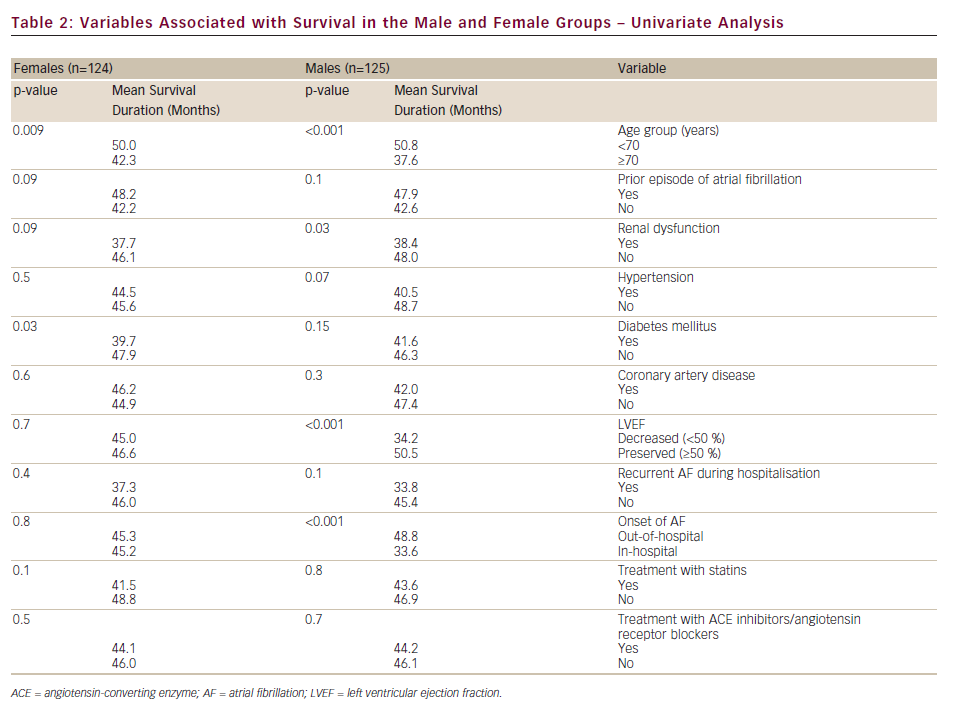
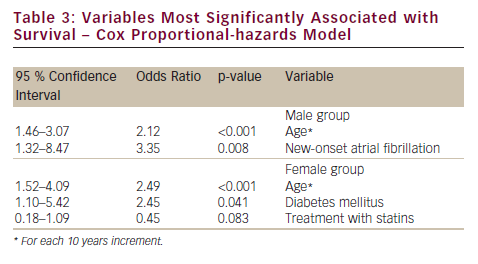
Table 2 depicts the variables associated with survival, as evaluated by univariate analysis. Age was significantly associated with poor survival in both groups (p<0.01). In the male group, renal dysfunction (p=0.03), decreased LVEF (p<0.001) and in-hospital onset of AF (p<0.001) were significantly associated with shorter survival. Diabetes mellitus was found significantly associated with decreased survival in women (p=0.03).
According to the results of multivariate analysis (see Table 3), age remained significantly associated with poor prognosis in both genders. However, for males, new onset AF (versus history of prior AF episode) was the variable most significantly associated with low survival. By contrast, for females, diabetes mellitus was associated with shorter survival, while treatment with statins predicted better prognosis.
Discussion
Characteristics of the Patients
In our prospective study we investigated gender-related differences in demographic, clinical, laboratory, electrocardiographic and echocardiographic data in patients with paroxysmal/persistent AF in an internal medicine ward. We confirmed the previous observations that compared to men, women with AF were older,4−14 more symptomatic,6,9,12,14 more likely to have hypertension,6,9−14 to be treated with calcium channel blockers13,14 or diuretics,8,13 and less likely to be smokers4,7,8,10,13 or to have abnormal LVEF.8−12 On the other hand, both gender groups were similarly treated with anticoagulants, antiplatelet agents and other relevant medications.6,11,13 In the present study, as compared the previous reports, the selection of the analysed variables was more extensive. Some of the observations are novel and may be of clinical importance. Thus, significant gender-related differences were found with respect to the laboratory data. Compared to the male group, our females demonstrated higher levels of cholesterol and ESRs as well as lower haemoglobin concentrations. One might speculate that a significant confounder of these differences might have been the post-menopausal state of a part of the female group. No significant differences between the groups were observed with respect to the rates of conversion of AF to sinus rhythm, recurrent episodes of AF during hospitalisation, meantime from onset to termination of AF and duration of hospital stay. Some of these findings are in contrast to a handful of reports published more than a decade before. In those studies, the increased risk for longer17 or recurrent18 episodes of paroxysmal AF was found in women, compared to men. The apparent discrepancy between the findings can be easily explained by profound changes in the modern management of AF.
Survival
We investigated a long-term survival, and the variables associated with the latter, separately in men and women. We found that on the 39-month median follow-up period all-cause mortality was comparable between the groups. Our observation is in contrast to a number of studies performed about a decade ago, reporting higher mortality in females versus males with AF.4,5,7 However, our results are consistent with the recently published data, wherein mortality rates at years one, two, five and 10 were found similar in both genders.8,9,11,14 Information regarding the gender-related differences in the impacts of various clinical variables on mortality of patients with AF is scarce. In the RACE study, women with recurrent persistent AF, who were randomly assigned to rhythm control, demonstrated significantly increased mortality as compared to those assigned to rate control.9 This difference was not observed in men. Hypertension, coronary artery disease and valve disease were associated with poor prognosis only in males.9 In a small study performed on outpatients with paroxysmal, persistent or permanent AF, age was the variable most significantly associated with five-year mortality in both genders.5 Other variables associated with increased mortality were treatment with angiotensin-converting enzyme inhibitor in males, and hypothyroidism and diabetes mellitus in females.5 We evaluated the impact of additional, not yet investigated, clinical variables on survival in hospitalised patients with paroxysmal or persistent AF, and found that significant predictors of death were different between men and women. It is not surprising that older age was associated with poor prognosis in both groups. Age is a known risk factor for mortality in patients with AF.5,19−22 However, we found that compared to the recurrent AF history, the new-onset AF was most significantly associated with low survival only in males. Association of first AF episode with poor prognosis has been reported in various patient populations.19,21,23 However, the possible association of increased mortality in the new-onset AF with gender has not been previously reported. It has been suggested that new-onset AF is a marker for the presence and severity of a previously unknown underlying disease.21 Moreover, increased mortality after the first episode of AF may be resultant from the worsening of cardiac function inflicted by the new-onset AF.23 These suggestions are supported by our echocardiographic data. Thus, in our male group the proportions of patients with decreased LVEF and segmental wall motion abnormalities were significantly greater, compared with the female group. It seems plausible that more careful evaluation of the patient as well as optimisation of the relevant treatment may be beneficial for men with first episode of AF.
With respect to the females, diabetes mellitus was associated with shorter survival, while treatment with statins predicted better prognosis. Diabetes mellitus is a known predictor of morbidity and mortality in AF.20,21,24 Poor prognosis in diabetic patients with AF results from older age, higher prevalence of co-morbidities and increased risk of cardiovascular events.24 In our patient population, diabetes was the most significant marker for shorter survival in women only. Increased mortality in diabetic women, compared to diabetic men, has been previously reported in patients with acute myocardial infarction25 and ischaemic stroke.26 Moreover, similarly to our results, in a study including 129 patients with AF, diabetes was found to be associated with increased five-year mortality, only in females.5 It was hypothesised that increased mortality in diabetic women may be due to increased risk for development of coronary artery disease and heart failure as well as high prevalence of hypertension and obesity.5,25,26 It is conceivable that diabetic females with AF might benefit from more strict control of cardiovascular risk factors, which hopefully would improve their survival.
Favourable effects of statins on AF have been previously reported. Use of statins was found to be associated with decreased risk of incidence and recurrence of AF after electrical cardioversion, cardiac surgery and acute coronary syndrome.27−29 In addition to cholesterol-reducing properties, statins positively affect the course of AF, due to their anti-inflammatory and antioxidant effects, attenuation of atrial remodelling and ion channel stabilisation.27–29 Surprisingly, there is a paucity of data concerning the impact of statin treatment on mortality in patients with AF. In the recent Japanese Rhythm Management Trial for Atrial Fibrillation (J-RHYTHM) study, post hoc analysis revealed no association between use of statins and survival in 823 patients with paroxysmal AF.22 Primary and secondary prevention studies involving patients free of AF reported that statins reduce the risk of cardiovascular events in women and men to a comparable degree.12,30 More so, studies that do report some gender-specific differences in pharmacokinetics of statins demonstrate a rather negative influence of statins on female populations compared to men.12,30 Thus, plasma concentrations of statins and risk of their adverse reactions have been found higher in women than in men.12,30 In general, statins are administrated less frequently in women than in men.12,30 Gender-related association of statin treatment with survival in AF patients has not been previously investigated. We have found that administration of statins was comparable in both gender groups (52 % of females versus 42 % of males) but was associated with better survival in the female group only. Since in our study the mean values of cholesterol and ESR were significantly higher in female participants as compared to males, it is possible that the cholesterol-lowering and anti-inflammatory effects of statins were more pronounced in women. It also cannot be ruled out that some other, yet unknown, mechanisms might be responsible for the beneficial impact of statins on survival in women with AF. This observation calls for performance of additional randomised studies aiming to more extensively evaluate the effect of statin treatment on mortality in patients with AF.
Study Limitations
The main limitation of the present study is the relatively small number of patients, which might have compromised our ability to define any other variables predictive of lower survival. It is also possible that our results were affected by the inclusion of patients from only one internal medicine department from a single medical centre, as well as by the specificity of local medical services.
Conclusions
We have found significant gender-related differences in clinical, laboratory and echocardiographic characteristics, as well as in survival predictors, in patients with AF hospitalised at an internal medicine ward. These results may be clinically important. They indicate that males with new-onset AF and females with diabetes mellitus require more optimal management in order to improve their long-term survival. Administration of statins to AF patients, especially to women, may be beneficial in terms of decreased mortality.