Angina pectoris and ischaemic heart disease have fascinated physicians in general and cardiologists in particular for decades. In today’s era of precision medicine, the challenge remains to correctly interpret the patient’s symptoms and determine the underlying (cardiac) cause. This provides the basis for adequate and appropriate treatment strategies. It is why the traditional concept of ischaemic heart disease focusing on epicardial atherosclerotic stenoses only is now outdated.
The spectrum of ischaemic heart disease is broad and encompasses several epicardial pathologies such as atherosclerotic disease, spontaneous coronary dissection and coronary spasm as well as microvascular abnormalities, such as microvascular spasm, impaired microvascular vasodilatation and increased microvascular resistance. The complex interplay between epicardial vessels and microvessels under physiological and pathophysiological conditions (so-called coronary autoregulation) should be appreciated.
In this context, the aim of the present article was to summarise contributions to the ESC Congress 2021 in the field of MI with non-obstructive coronary arteries (MINOCA) and angina with non-obstructive coronary arteries (ANOCA). This may help in opening up new avenues of research and clinical care for our patients.
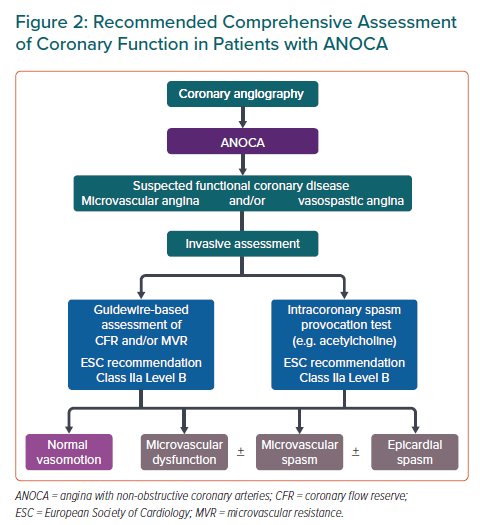
In recent years, the clinical scenario of patients with MINOCA has received increasing attention. A diagnostic algorithm for MINOCA patients was published in the 2020 European Society of Cardiology (ESC) guidelines on non-ST-elevation MI (NSTEMI) and the so-called traffic-light approach should be followed to reach a final diagnosis in these patients (Figure 1).1
Several studies presented at the ESC Congress 2021 assessed the prognosis of patients with MINOCA. Hinrichs et al. assessed and compared the prognosis of 1,704 patients who had type 2 MI, patients with type 1 MI (n=1,699) and those without MI (total n=14,883) from Germany.2
Type 2 MI was defined as a significant troponin increase without percutaneous coronary intervention. During a mean follow-up of 3.4 ± 3.6 years, 3,321 deaths occurred (18.2%). Compared to patients without MI (16.1%), patients with type 1 MI (25.2%) and type 2 MI (29.1%) had significantly higher mortality rates (p<0.001). Kaplan–Meier analysis confirmed the lowest survival rates occurred in patients with type 2 MI.2
Moreover, Barrett et al. showed that 1,544 MINOCA patients from Israel had a favourable short-term outcome but their long-term outcome was comparable to that of patients with acute MI due to obstructive coronary artery disease.3
In addition, in a study including 712 Spanish patients with acute coronary syndrome (ACS), Espinosa Pascual et al. highlighted that pro-inflammatory states such as autoimmune pathologies, connective tissue disease, active cancer and infections should be regarded as risk factors for the occurrence of MINOCA.4
Therefore, the prognosis of MINOCA patients is not as good as previously thought and establishing a final diagnosis as the cause for the event should be pursued to initiate the most appropriate treatment.
One important MINOCA subtype is that arising from coronary spasm. Pirozzolo et al. showed that patients with MINOCA due to coronary spasm (determined by acetylcholine provocation testing) had a worse prognosis than MINOCA patients with an uneventful spasm test.5 Ninety-six patients with MINOCA were followed up for a median of 5 years. Patients with coronary spasm on acetylcholine testing (n=51) had a significantly worse prognosis regarding death from any cause and MI during follow-up then those with an uneventful spasm test (n=45).
Montone et al. showed that acetylcholine provocation testing in patients with either chronic coronary syndrome or acute coronary syndrome is safe and that the test itself does not affect long-term prognosis.6 This should reassure clinicians and interventionists that they can proceed with such tests to establish a clear diagnosis followed by targeted treatment.
Another MINOCA subtype are patients with spontaneous coronary artery dissection (SCAD). These are often younger, female patients and they are frequently undiagnosed. However, Elkaryoni et al. showed that in-hospital mortality of 338 patients with SCAD was comparable to that of 17,218 non-SCAD ST-elevation MI (STEMI) patients.7
Furthermore, Mori Junco et al. showed that a specific angiotype of SCAD – a circumscribed contained intramural haematoma – was associated with an increased risk of short-term adverse clinical events that persisted during follow-up.8 This underlines that interventionists should be familiar with the angiographic classification of SCAD, and additional intravascular imaging may be needed in cases with diagnostic uncertainty.9
A working diagnosis of MINOCA is also frequently given to patients who are finally diagnosed with takotsubo syndrome. Although this syndrome has been classified as non-ischaemic in the traffic-light approach, debate is ongoing over whether this is correct. Studies have shown that coronary spasm and microvascular dysfunction are, indeed, present in patients with takotsubo syndrome, suggesting that a vascular dysfunction leading to myocardial ischaemia may be involved in the syndrome.10–12
At ESC 2021, a study by Bonanni et al. shed new light on the molecular profile of patients with takotsubo syndrome. This showed that these patients (in comparison to those with STEMI due to obstructive coronary disease) had significantly higher gene expressions for nitric oxide synthase 3, superoxide dismutase 1 and transferrin receptor, all of which are involved in oxidative stress pathways.13
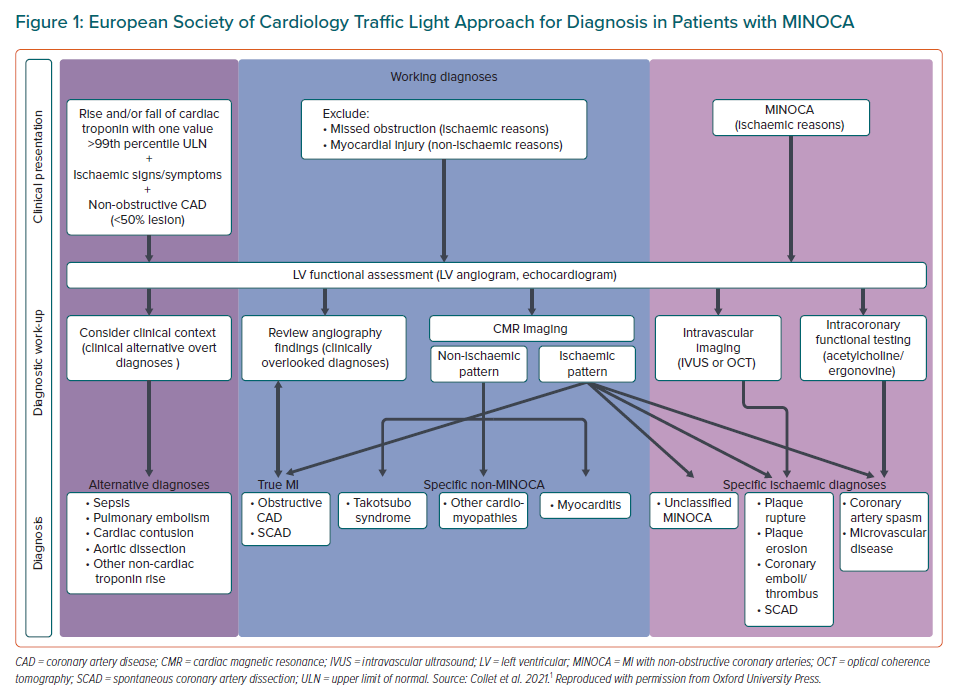
Patients with ANOCA are equally heterogeneous as those with MINOCA and several endotypes have been defined.14 A study by Toya et al., assessing coronary flow reserve and hyperaemic microvascular resistance using adenosine in patients with ANOCA, showed that coronary flow reserve was predictive of outcomes in men whereas hyperaemic microvascular resistance was predictive of outcomes in women.15 This study highlights the importance of comprehensive diagnostic assessments in patients with ANOCA as recommended by the ESC 2019 guideline on chronic coronary syndromes.16
Invasive assessments for coronary spasm using provocation testing have a Class IIa recommendation as invasive measurements of coronary flow reserve and microvascular resistance (Figure 2).
Although coronary spasm is much more frequent in ANOCA patients than impaired microvascular vasodilatation (i.e. diminished coronary flow reserve or increased microvascular resistance), the latter is a strong prognostic marker, as recently shown by Kelshiker et al.17,18
Ejupi et al. investigated proteomics in patients with ANOCA and found that several biomarkers were associated with vascular dysfunction in these patients, with little overlap between different endotypes.19 This underscores the need for more multidisciplinary research in this area in search of new pharmacological targets and the potential application for diagnostic purposes.
In summary, the field of MINOCA and ANOCA is evolving and, apart from comprehensive diagnostic assessments in clinical routine, randomised studies on pharmacological treatments in patient subtypes are eagerly awaited.