Myocardial bridging (MB) is a congenital coronary anomaly in which a segment of a coronary artery traverses through the myocardium for a portion of its length.1 Despite being asymptomatic in most people, some data suggest that it might be responsible for myocardial ischaemia and angina.2–5 The possibility for MB to cause myocardial ischaemia, however, is questioned because it only causes reduction or interruption of coronary blood flow during systole, as a result of compression of the intramural tract of the vessel by myocardial contraction, while most myocardial perfusion (>85%) occurs in diastole when blood flow through the bridged coronary segment is restored. Several mechanisms have been proposed for the possibility that MB can induce myocardial ischaemia.1,5–10 However, there is a lack of convincing evidence and clinical data to support the induction of myocardial ischaemia by MB. Thus, the aim of this study was to obtain further insights into whether the dynamic coronary stenosis/occlusion related to MB can cause myocardial ischaemia, as assessed by abnormalities in systolic and diastolic function of the left ventricle during maximal electrocardiographic and echocardiographic exercise stress testing.
Methods
Patients
We reviewed the results of all invasive coronary angiographies performed at our university hospital between January 2018 and June 2022 to identify patients who fulfilled the following inclusion criteria: evidence of MB; normal coronary arteries, defined as the absence of any coronary stenosis ≥20% of the vessel lumen diameter; aged between 30 years and 80 years.11
The patients’ clinical records were reviewed and those with evidence of any of the following conditions were excluded: any other significant form of heart disease, such as valvular or cardiomyopathy; a cardiac rhythm other than sinus, such as AF or pacemaker; history of severe non-cardiac disease, such as acute and/or chronic inflammatory diseases, autoimmune diseases, neoplastic diseases or renal or liver dysfunction; inability to perform exercise stress test; and suboptimal echocardiographic windows as described in echocardiographic reports.
A group of consecutive patients who underwent invasive coronary angiography because of symptoms suspected of ischaemic heart disease, but who were found to be free of any coronary abnormality, including MB, and were also known to have normal results at non-invasive stress tests (ECG and/or radionuclide stress test) were identified and served as a control group.
The study protocol was approved by our institutional review board and the identified patients and controls were invited to participate in the study after being given full information about the scope and methods of the study. A signed written informed consent was obtained from each patient who agreed to participate.
Exercise Stress Test
All patients underwent a treadmill exercise stress test (EST) under ECG monitoring and a complete echocardiographic examination was performed at rest and at peak exercise.
EST was performed by a standard Bruce protocol under continuous monitoring of three ECG leads (DII, V2, V5). A standard ECG was printed at rest, at the end of each stage, at peak exercise, at 1-minute intervals in the recovery phase and when it was thought to be clinically indicated, for example, when ST-segment depression, symptoms or arrhythmias were found. Blood pressure was measured at each stage.
The test was interrupted only in case of: fatigue or the patient wanted to stop; occurrence of important symptoms such as angina or dyspnoea; clinically relevant ECG changes, such as ST-segment depression ≥4 mm, ST-segment elevation ≥2 mm, complex ventricular arrhythmias; a decrease in blood pressure below the values measured at rest; a value of systolic blood pressure ≥240 mmHg and/or diastolic blood pressure ≥130 mmHg.
The ECG was considered positive for the occurrence of myocardial ischaemia when a horizontal or downsloping ST segment depression ≥1 mm was detected in one or more ECG leads, persisting for 60–80 ms after J point.
Echocardiographic Examination
A standard echocardiogram was performed before EST and immediately after peak EST by an expert echocardiographer using a Toshiba Artida echocardiographic machine equipped with a 3.5 MHz sector probe, with simultaneous monitoring of a single electrocardiographic lead. Images and videos were stored on our institutional database and subsequently separately analysed by two expert echocardiographers who were blinded to patient group and exercise ECG results. They used the TomTech software following international recommendations.12,13
Left ventricle (LV) systolic function was assessed by measuring LV ejection fraction (LVEF) from four-chamber and two-chamber apical views by the Simpson biplane method. Regional systolic function was assessed according to the 17-segment model and a 1–4 score classification (1=normal; 2=hypokinetic; 3=akinetic; 4=dyskinetic). A global and regional wall motion score was obtained by adding the individual segment scores.
LV diastolic function was checked by obtaining the E/A and the E/e’ ratios.14 To obtain the E/A ratio, the trans-mitral flow was visualised by colour Doppler and recorded by pulsed-wave Doppler by positioning the sample volume at the level of the coaptation point of mitral valve flaps in apical four-chamber view; the E and A wave peaks were measured and the E/A ratio was derived. The longitudinal excursion of the LV myocardium near the mitral annulus was assessed by tissue-Doppler, placing the sample volume both at the level of the septum and the lateral wall and the e’ wave was obtained. Then, the septal and lateral E/e’ ratios were calculated and the average E/e’ ratio was used for analyses.
Finally, speckle-tracking echocardiography (STE) was performed and LV global longitudinal strain (GLS), which represents the shortening of myocardium along its longitudinal axis and has been shown to be more sensitive than LVEF in identifying initial LV dysfunction, was calculated at rest and peak EST.15,16 GLS was measured on frame loops of at least three consecutive cardiac cycles recorded in 2D apical scan projections in four-chamber, two-chamber and three-chamber views, applying the formula:
ε=(L−L0)/ L0),
where L-L0 is the variation in length and L0 the basal length. Longitudinal strain (LS) was also calculated for the basal, medium and apical segments of the anterior and inferior wall. According to its formula, LS is usually reported as a negative value; however, in this article, data are reported as absolute (positive) numbers to facilitate comprehension and discussion.
Statistics
Continuous variables are expressed as means with standard deviations and were compared by analysis of variance. Nominal variables are expressed as numbers and percentages and were compared by Fisher’s exact test. The changes at peak EST compared to baseline of echocardiographic parameters were assessed by a linear general model with a repeated measure design. Within-group comparisons were done by paired t-test in case of significant differences in the group variable interaction. All analyses were performed using SPSS 28.0. A p-value of <0.05 was required for statistical significance.
Results
Characteristics of Patients
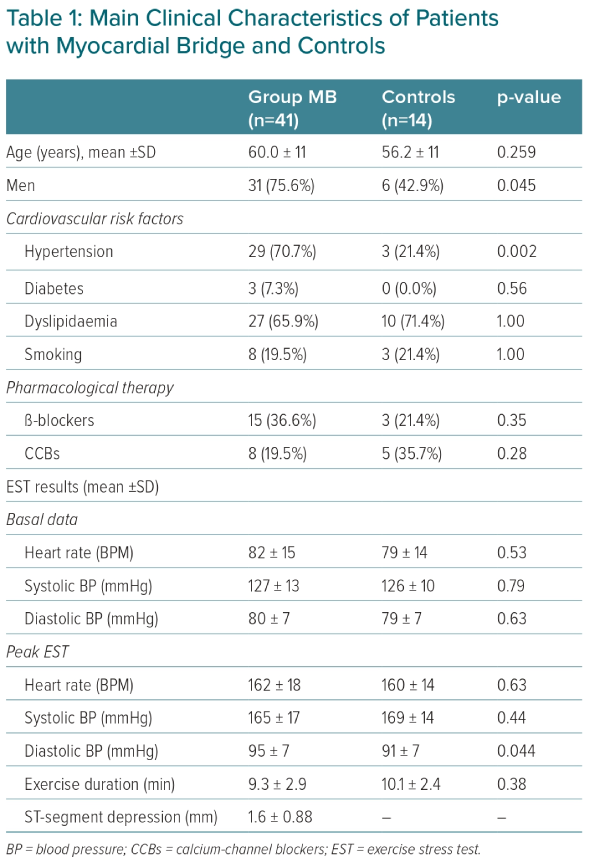
The study included 55 patients – 41 (mean age 60 ± 11 years; 31 men) with MB and 14 control patients (mean age 56 ± 11 years; six men). The main clinical characteristics of the two groups are summarised in Table 1. Patients with MB included more men p=0.045) and hypertensive (p=0.002) subjects, but there were no other statistically significant differences between the two groups.
MB in the study group involved the mid-part of the left anterior descending (LAD) coronary artery in 36 patients (88%), while the distal part of the LAD coronary artery was involved in four patients (10%). Both the mid- and distal parts of the vessel were involved in one patient (2%).
Exercise Stress Test
The main results of EST in the two groups of patients are summarised in Table 1. There were no differences in baseline heart rate (HR), systolic blood pressure (SBP) and diastolic blood pressure (DBP). Exercise duration and peak HR and SBP were also similar in the two groups, whereas peak DBP was slightly higher in the MB group compared to controls (p=0.044).
A positive EST (ST-segment depression ≥1 mm) was found in 18 patients of the MB groups (43.9%), whereas no control subject developed significant ECG changes during EST (p=0.001). ST depression in MB patients with positive EST was 1.57 ± 0.76 mm (range 1–3 mm).
Echocardiographic Stress Test
The main echocardiographic findings observed at rest and peak EST are shown in Table 2. At baseline, standard echocardiographic parameters were normal in both groups and there were no significant differences between them. During exercise, LVEF improved significantly in both groups with no statistically significant difference (p=0.09) and in the absence of any segmental wall motion abnormalities in both groups.
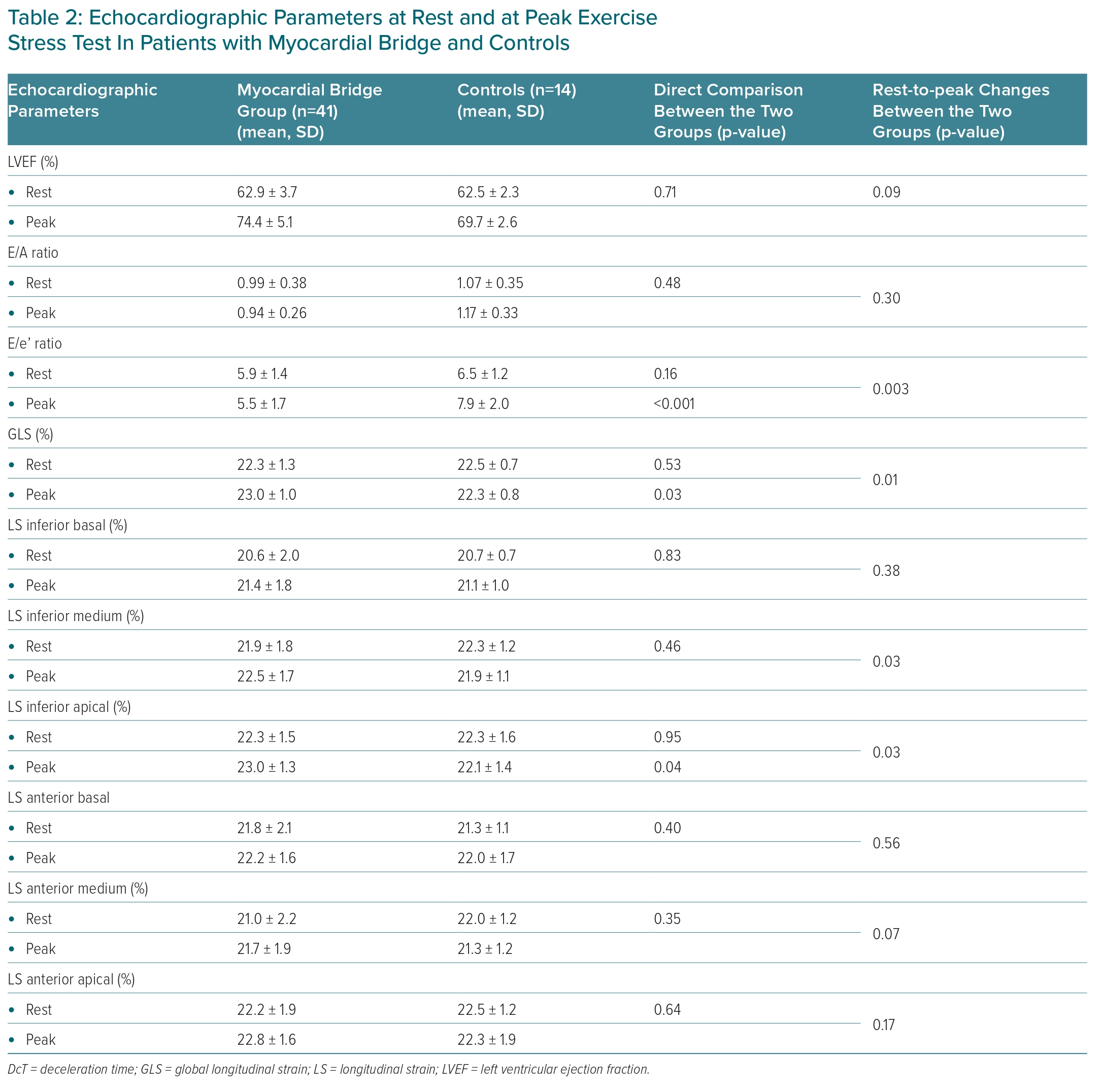
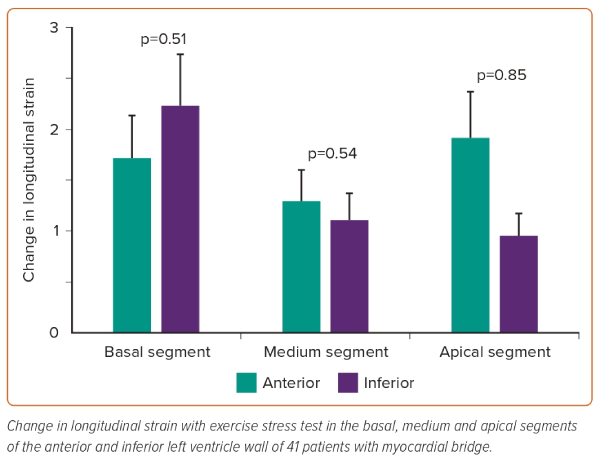
Detailed data of GLS and regional LSs are also summarised in Table 2. At rest, both GLS and regional LS did not show any significant differences between the two groups. Changes in GLS due to exercise were significantly different between the two groups, with GLS showing a trivial reduction in controls but a small increase in MB patients (p=0.01). Similar trends were found for regional LSs that reached statistical significance for the medium (p=0.028) and apical (p=0.032) segments of the inferior wall.
Importantly, in MB patients the changes to LS in the basal, medium and apical segments of the anterior wall were not significantly different compared with those detected in the corresponding segments of the inferior wall (Figure 1).
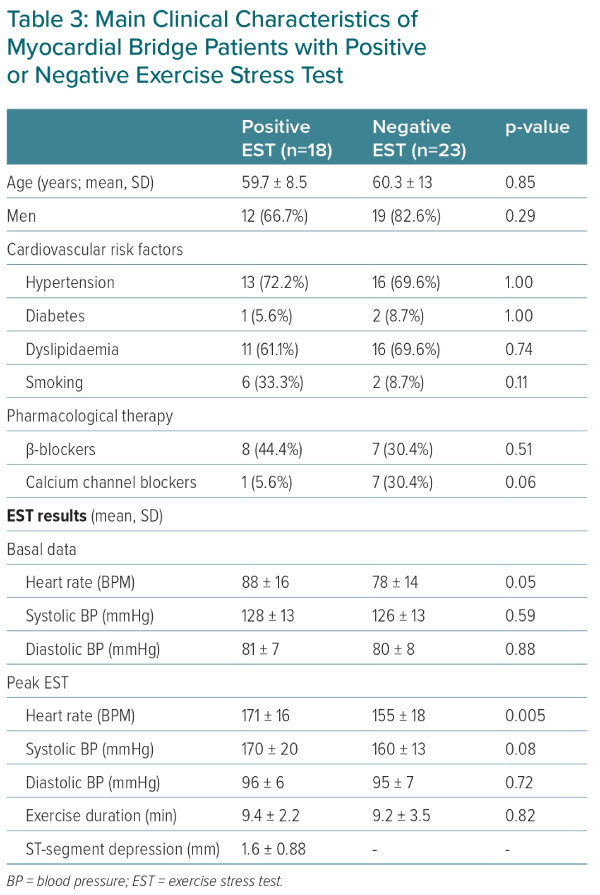
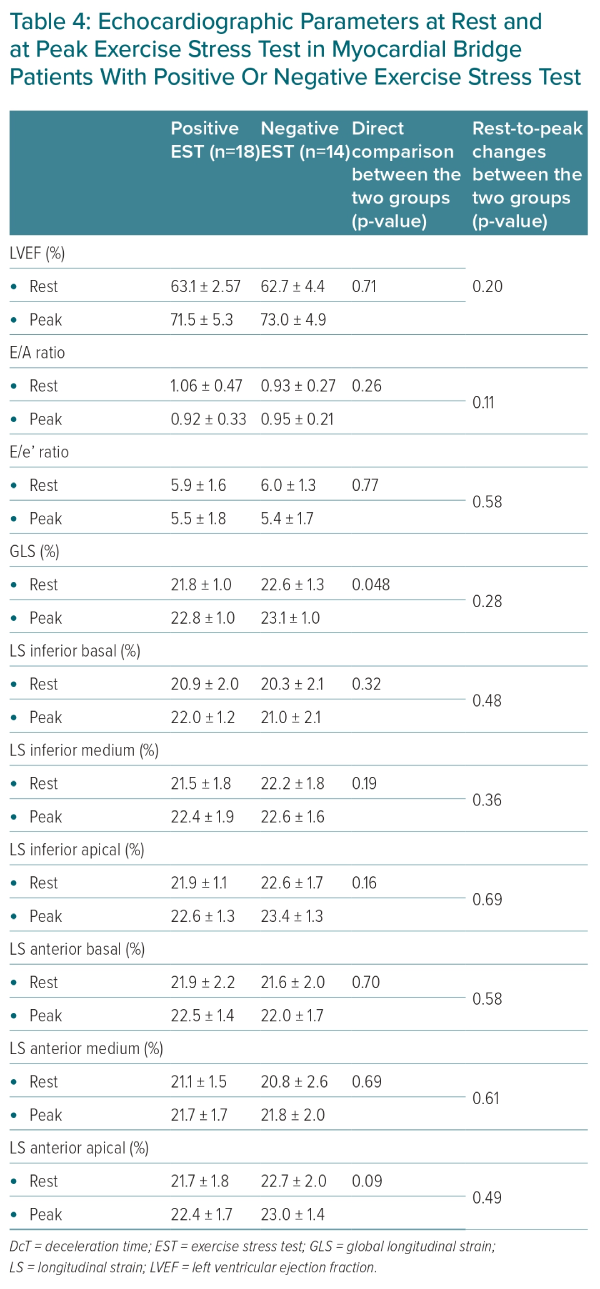
Relation between ECG and Echocardiographic Results
In the MB group, 18 patients (43.9%) developed significant ST-segment depression during EST (see above). The main clinical characteristics and EST findings of MB patients with positive versus negative EST are summarised in Table 3, whereas echocardiographic results of these two groups are shown in Table 4. Clinical features were similar in these two subgroups, although more patients were treated with calcium-channel blockers among those with a negative test (p=0.059). EST parameters were also similar in most aspects, but patients with a positive test had a higher heart rate both at rest and at peak exercise. Most echocardiographic data showed similar changes with EST in the two groups of MB patients. In particular, GLS showed a significant improvement at peak exercise compared to baseline with no difference between the two groups. Similar results were observed for regional LS (Table 4).
Discussion
The novel finding of this study is that MB detected at coronary angiography is unlikely to be a usual cause of exercise-induced myocardial ischaemia, even in the presence of ischaemic ECG changes.
The detection of normal coronary arteries in patients with angina chest pain and exercise-induced ECG changes typical enough to suggest obstructive coronary artery disease is a challenging diagnostic issue. In most cases, no immediate anatomical causes can be found, usually prompting the search for coronary microvascular dysfunction and/or coronary artery spasm, which are relevant causes of the symptoms in these patients.17,18 A proportion of these patients show the presence of MB at invasive coronary angiography and/or coronary CT, suggesting a pathogenetic role in the ischaemic picture of the patient.1
However, whether MB results in myocardial ischaemia in clinical practice remains controversial. The impairment of coronary blood flow by MB mainly occurs during the systolic phase of the cardiac cycle, which usually results in negligible effects on myocardial perfusion, which mainly occurs during diastole (85% of myocardial perfusion/flow). Thus, although several theories and some clinical pathophysiological studies have supported the possibility for MB to trigger ischaemic events in individual patients, including slow recovery of diastolic flow through the compressed vessel and susceptibility to coronary spasm of the bridged segment, the ischaemic burden of MB in clinical practice remains poorly defined.1–10
In this study, we failed to demonstrate any significant ischaemic impairment of LV systolic and diastolic function at maximal EST in patients with documented MB as compared with similar patients with normal/near normal coronary arteries but without MB at coronary angiography.
We failed to demonstrate a stress-induced impairment of a very sensitive echocardiographic parameter of subclinical LV dysfunction, such as both global and segmental LS, including LS of the medium and apical anterior segments, perfused by the bridged coronary artery. We also found no evidence of LV dysfunction during EST among patients with MB who developed ECG signs of myocardial ischaemia during EST (n=18, 43.9%), as compared to those without ECG evidence of myocardial ischaemia during the test.
The ischaemic ECG changes in these patients are, therefore, unlikely to be caused by MB of the LAD. If MB were responsible for ischaemic ECG changes, this should have resulted in some wall motion abnormality in at least some patients at echocardiography due to the rather extensive myocardial territory perfused by the LAD. The lack of even subtle abnormalities in myocardial function, instead, rather suggests ischaemic ECG changes probably resulted from coronary microvascular dysfunction, a frequent cause of myocardial ischaemia with non-obstructed coronary arteries (INOCA), which is notoriously associated with the lack of wall motion abnormalities due to its patchy distribution in the myocardium, a hypothesis that is supported by results of a recent study (see below).19,20
Thus, our data question the ability of MB to trigger significant degrees of myocardial ischaemia, at least in most patients with this abnormal finding detected at angiography.
Our data are at variance with those of some previous studies. Lin et al. reported a specific abnormality induced during exercise echocardiography in 18 patients with MB of the LAD coronary artery detected by IVUS consisting in a mid-septal buckling in the end systolic to early diastolic phase of the cardiac cycle, also showing an association of the abnormality with a reduced diastolic fractional flow reserve (FFR, ≤0.75) within and/or distal to the bridge, as measured during dobutamine challenge.3 The same group subsequently reported a lower septal LS at peak exercise echocardiography in 58 patients with MB of the LAD coronary artery, detected by IVUS, compared to 50 matched healthy controls (18.9% ± 2.6% versus 21.7% ± 1.6%; p<0.001), whereas there was no significant difference between the two groups in lateral LS. Of note, diastolic FFR throughout the MB during invasive dobutamine challenge was a major predictor of the lower changes in septal LS during exercise echocardiography.21
In a smaller study involving 18 patients with MB, Jhi et al. found lower LS and radial strain during dobutamine echocardiography test in the anterior and antero-septal segments of the myocardial wall as compared with posterior segments, also identifying a dyssynchronous pattern of septal segments.22 Finally, in a study involving 92 patients with angina and non-obstructive coronary artery disease, Sinha et al. reported impairment of coronary flow reserve in 30 patients (33%) who had evidence of MB, which seemed mainly related to a reduced accelerating wave energy in early systole of perfusion efficiency.23 However, there seemed to be no significant differences in coronary flow reserve and accelerating wave energy in early systole of perfusion efficiency between patients with MB and 33 patients (36%) who had evidence of coronary microvascular dysfunction but not MB, thus questioning whether myocardial ischaemia in MB patients was actually related to MB rather than to concomitant coronary microvascular abnormalities.20 The clinical presentation of patients in whom myocardial ischaemia is shown to be clearly caused by coronary microvascular dysfunction, is similar to that of patients with evidence of MB at invasive angiography or coronary CT. Of note, whether MB may in some way favour coronary microvascular dysfunction or it is just an innocent bystander in these patients remains to be elucidated.
The reasons for the differences between previous studies and ours are not completely clear. Patient selection and methods used to detect MB and perform stress testing might play a role. However, in all studies that assessed LV strain, including ours, the changes in LV strain during EST seem modest, thus making it difficult to exclude that the differences observed among studies might simply be related to chance, but also suggesting that the clinical implications of MB are likely to be of little consequence at best.
Study Limitations
Some limitations of our study should be acknowledged. First, we did not perform a sample size calculation to include a number of patients that allowed an adequate statistical power. We cannot exclude, therefore, that the number of patients included in the study was insufficient to detect some effects on myocardial ischaemia by MB. Therefore, our data need to be confirmed in larger studies with established statistical power. Second, we only correlated the presence of any type of bridge with the effects on global and segmental LV-LS during EST. Thus, we cannot exclude that the selection and assessment of a large population of patients with more severe forms of MB, such as deep and/or long segments, might reveal some ischaemic effect during exercise stress conditions in at least some patients, which has been suggested by previous reports.21 Third, we acquired stress echocardiographic imaging after peak exercise and therefore, we cannot completely exclude that a very transient abnormality might have been present between peak exercise and image acquisition; however, echocardiographic images were acquired within 30 seconds from peak EST and therefore any undetected very transient myocardial dysfunction would be of questionable clinical relevance. While our data tend to exclude significant exercise-induced myocardial ischaemia induced by MB, we cannot exclude that the latter may favour myocardial ischaemia by other types of mechanisms, independent of exercise and increase in myocardial oxygen demand, such as coronary constriction/spasm at the level of MB.
Conclusion
Although further studies are welcomed to further characterise the effects of MB on myocardial perfusion, our data do not support the notion that MB results in significant degrees of myocardial ischaemia as assessed by LV systolic and diastolic function during maximal EST. 
Clinical Perspective
- Our study shows that the presence of myocardial bridge is not associated with clear evidence of myocardial ischaemia during echocardiographic stress tests.
- This occurs despite the evidence of ischaemic electrocardiographic changes during the stress test.
- Our data suggest that patients with myocardial bridge can usually be reassured about the risks of ischaemic events related to physical exercise.