Sports-related sudden cardiac death (SCD) is a rare but devastating consequence of sports participation. While its exact incidence remains elusive and varies with geographic localities and sports genre, available evidence suggests an overall incidence of between 1 in 50,000 and 7 in 100,000 per year in healthy young athletes (<35 years old).1–3 An 11-year review in Singapore found that 87% of sports-related sudden death in athletes were due to SCD.4 It should be noted that sport per se is not the cause of SCD in athletes. Rather, the presence of an underlying cardiovascular abnormality is the primary substrate upon which intensive physical exercise acts as a trigger for the athlete to develop SCD.
Given the threefold increased risk of SCD among athletes and the intense cardiovascular and cardiopulmonary demands required by training and competition, multiple guidelines have recommended pre-participation screening to identify at-risk athletes and provide appropriate medical advice for these athletes.5 In general, the most frequent pathological findings in SCD among young athletes aged <35 years in the Western world, either from survivors or from post-mortem series, are hereditary or congenital structural and electrical cardiovascular abnormalities. These include – but are not limited to – hypertrophic cardiomyopathy, arrhythmogenic cardiomyopathy and coronary artery anomalies, premature coronary artery disease, abnormal vascular conditions related to connective tissue diseases such as Marfan syndrome, and channelopathies.6,7 The prevalence of such latent cardiovascular conditions, which may be unmasked or aggravated during strenuous physical training or competitive events, has led to the formulation of guidelines, along with cardiac and sports medicine professional societies worldwide recommending selective pre-participation screening to identify at-risk athletes, and subsequently to provide appropriate medical advice and assessment for further participation.1,8–13
However, epidemiological data from Asia remain incomplete or unavailable.4 While the Asia-Pacific region (comprising Asia, Western Pacific and Oceania) makes up slightly over one-third of the global landmass, it contains over 60% of the world’s population. This implicitly extrapolates to significantly more young athletes from these countries when compared with the rest of the world.14 Moreover, several differences exist between the Asia-Pacific and the West in terms of sports type, level of participation and the epidemiology of cardiovascular disease. Firstly, the types of sporting activities within Asia differ substantially from Western countries. Many martial arts are popular in Asia and these combat sport disciplines bear the potential risk for commotio cordis as a cause of SCD.14–17 Secondly, the prevalence of predisposing conditions such as arrhythmogenic cardiomyopathy, Brugada-type ECG patterns, Kawasaki disease, rheumatic heart disease and coronary artery disease in the young have been reported to be higher in some Asian populations compared to non-Asian populations.18–24
Lastly, there is a disparity between countries in the Asia-Pacific region in terms of economics, health resources, health systems, and costs of and access to medical services, which may have a substantial impact on the implementation of programmes aimed at minimising the impact of sports-related adverse cardiovascular events. Hence, it may not be appropriate to adopt standards of care from the West in its entirety to the Asia-Pacific region without careful consideration and contextualisation of these issues. With these differences in mind, this consensus statement was developed with the aim to guide medical practitioners involved in the screening and care of young competitive athletes, with a focus on select issues pertinent to the Asia-Pacific region.
Methods
The Asian Pacific Society of Cardiology (APSC) convened a 20-member multidisciplinary expert panel of cardiologists and sports medicine specialists to develop a consensus statement to provide guidance on pre-participation cardiovascular screening in young competitive athletes. The panel comprised experts from France, Hong Kong, Indonesia, Philippines, Singapore, South Korea, Taiwan and Thailand. The experts of the panel are members of the APSC who were nominated by national societies and endorsed by the APSC consensus board or were invited as international experts. After a comprehensive literature search, the available evidence was then appraised using the Grading of Recommendations Assessment, Development, and Evaluation system.25 Using this system, the level of evidence was assigned as follows:
- High (authors have high confidence that the true effect is similar to the estimated effect).
- Moderate (authors believe that the true effect is probably close to the estimated effect).
- Low (true effect might be markedly different from the estimated effect).
- Very low (true effect is probably markedly different from the estimated effect).
The available evidence was then discussed, and consensus statements developed, during a consensus meeting held online in December 2020. Each statement was then voted on by each panel member using a three-point scale (agree, neutral or disagree), via online polling. Consensus was reached when 80% of votes for a statement were agree or neutral. In the case of non-consensus, the statements were further discussed via electronic communication, then revised accordingly until the criteria for consensus were reached.
For these consensus statements, young competitive athletes are defined as those younger than 35 years of age (no lower age limit) who participate in an organised team or individual sport that requires regular competition against others as a central component, places a high premium on excellence and achievement, and requires some form of systematic and usually intense training.26
Classification of Exercise and Sports Intensity
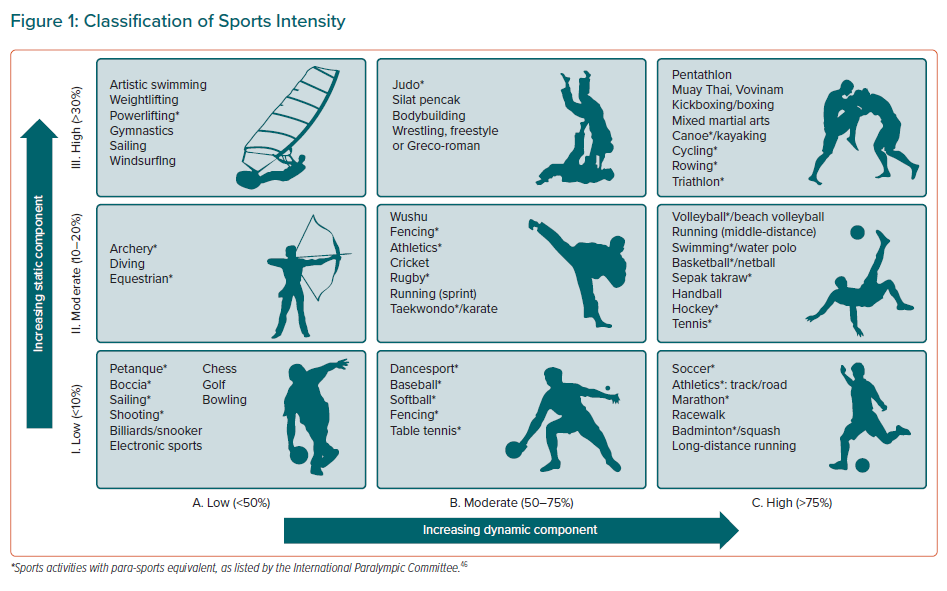
Due to the variable impact of intensity of physical activity on the risk of cardiovascular events in susceptible athletes, the expert panel classified various sports according to the gradated intensity of their static (I. Low; II. Moderate; and III. High) and dynamic (A. Low; B. Moderate; and C. High) components (Figure 1).27–29 This system was adapted from the established American Heart Association (AHA)/American College of Cardiology (ACC) classification.12,30 Specifically, competitive sports unique to the Asia-Pacific region were curated from the Commonwealth Games, Asian Games, Southeast Asian Games and the Paralympics to ensure not only inclusiveness but also that such sports indigenous to this part of the world are adequately highlighted.
In general, sports can be broadly dichotomised into static and dynamic elements. The static component is expressed as the relative intensity of static muscle contractions, while the dynamic component is reflected by the relative intensity of dynamic exercise (regular contraction of large muscle groups) or percentage of maximal aerobic power (VO2 max). Static contractions increase afterload; the greater the intensity of the contraction of skeletal muscles, the greater the rise in blood pressure and consequently the afterload on the left ventricle. Dynamic exercises primarily result in volume loading of the left ventricle. In this set of recommendations, a greater emphasis is placed on the dynamic component of sports because cardiorespiratory activity, as a function of maximal aerobic capacity, has been conventionally linked to adverse outcomes.31
Intuitively, this is congruent with haemodynamic principles, as increasing dynamic exercise intensities result in increased rate pressure product, flow states, and sympathetic tone, all of which are known triggers or aggravators of ischaemia, structural decompensation, and electrical instability in predisposed individuals – all with consequent downward spiral in haemodynamics.
For the purpose of these consensus statements, sports in the IA category (Figure 1) are considered low-intensity sports while IIA, IIB and IB sports are considered moderate intensity, with IC, IIC, IIIA, IIIB and IIIC making up the remaining sports that are placed in the high-intensity domains. This classification system aims to provide an approximate guide in estimating the intensity of the selected sports and is not meant to be prescriptive. The panel acknowledges that in real-world practice, static and dynamic intensities in any given sport do not occur as distinct categories, but rather along a fluid scale. Sports intensities can be highly variable throughout the training–competition continuum and are confounded by individual fitness, motivation and environment.
Consensus Statements
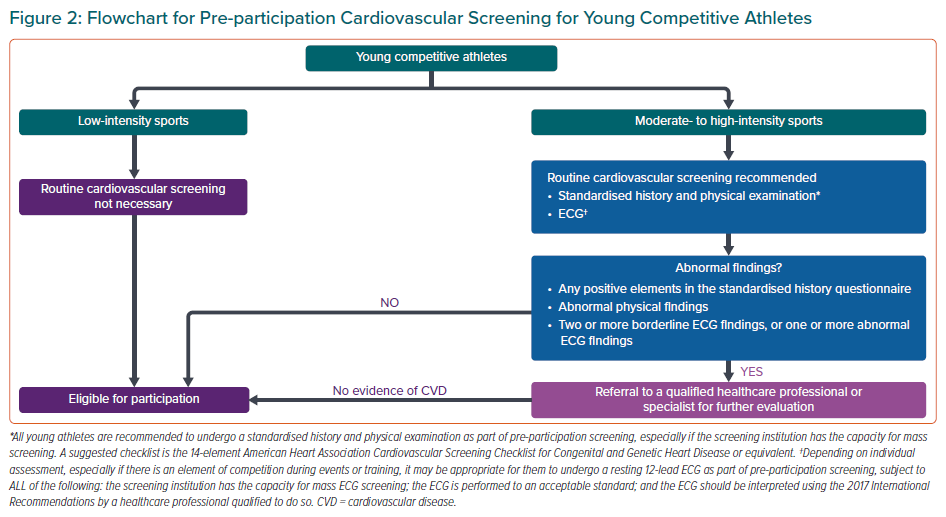
The expert panel developed three sets of statements for the pre-participation screening of young competitive athletes. Specifically these were for participation in high and moderate cardiovascular intensity sports, for participation in low-intensity sports and for athletes with pre-existing cardiovascular disease. The panel voted to converge the recommendations for high- and moderate-intensity sports to simplify the overall approach for pre-participation screening. Figure 2 shows a flowchart summarising these recommendations.
Participation in High and Moderate Cardiovascular Intensity Sports
Statement 1. Young competitive athletes are recommended to undergo a standardised history and physical examination as part of pre-participation screening, especially if the screening institution has the capacity for mass screening. A suggested checklist is the 14-element AHA Cardiovascular Screening Checklist for Congenital and Genetic Heart Disease or equivalent.
Level of evidence: Low.
Level of agreement: Agree 95%, neutral 5%, disagree 0%.
Statement 2. Young competitive athletes are recommended to undergo a resting 12-lead ECG as part of pre-participation screening, provided that all of the following are fulfilled:
- the screening institution has the capacity for mass ECG screening;
- the ECG is performed to an acceptable standard; and
- the ECG should be interpreted by a trained healthcare professional, with reference to prevailing standards.
Level of evidence: Low.
Level of agreement: Agree 100%, neutral 0%, disagree 0%.
Statement 3. Referral to a qualified and relevant healthcare professional/specialist for further evaluation should be considered in the presence of any of the following:
- any positive element(s) in the standardised history questionnaire, or
- abnormal physical finding(s) on physical examination, or
- two or more borderline findings on ECG, or one or more abnormal ECG findings (based on the International Recommendations 2017).
Level of evidence: Low.
Level of agreement: Agree 95%, neutral 5%, disagree 0%.
Where appropriate, a three-generation family history including sudden death, congenital heart disease, and premature cardiovascular disease and complications should be queried. As the risk of SCD is inherently elevated in sports of moderate and high intensity, routine pre-participation cardiovascular screening via standardised history-taking and physical examination must also be performed for young competitive athletes engaging in these categories of sports.27–29 Pre-participation screening allows the upstream identification of otherwise asymptomatic athletes who have underlying cardiovascular conditions that predispose them to SCD.32
As part of comprehensive medical history-taking for pre-participation, standardised checklists, including the 14-element AHA Cardiovascular Screening Checklist for Congenital and Genetic Heart Disease, can be implemented by any healthcare practitioner involved in sports screening.32 Such questionnaires include the presence or absence of suspicious symptoms (e.g. exertion-related symptoms), significant past medical history or prior sports restrictions, and family history of cardiovascular disease, especially inheritable conditions. A thorough physical examination of the cardiovascular system should also be conducted during the encounter to assess for features that may suggest underlying cardiovascular conditions that preclude participation (e.g. heart murmurs, frequent ectopic beats, pulse delays, physical stigmata of Marfan syndrome and sitting brachial artery blood pressure).33 Importantly, the thorough medical history-taking and physical examination are relatively affordable and easily accessible even in developing countries, thus imposing a low barrier to enable effective sports screening.
While medical history and physical examination constitute a useful first line of screening, there may have low sensitivity to detect latent cardiovascular diseases in the young because such conditions are often clinically silent, and unlikely to be easily detected during the initial clinical encounter.34 To improve the overall sensitivity of detection, the addition of a 12-lead ECG is recommended as a low-cost and widely available tool for the pre-participation screening of athletes involved in moderate- to high-intensity sports.1 As an add-on, the ECG can enhance the screening sensitivity of pre-participation screening from 25% to >90%, to pick up cardiovascular conditions that may predispose to SCD.32,35–37
A recent meta-analysis reported that the ECG was more sensitive than history and physical examination alone in detecting significantly underlying cardiovascular conditions related to SCD.37 A common criticism of ECG screening is the high false-positive rate, leading to either unnecessary secondary evaluations or restriction from sports activities. However, it is critical to recognise that the false-positive rate for ECG screening is largely affected by the criteria used to define ‘abnormal’. With significant advances made in interpretation of an athlete’s ECG, the ECG has improved the ability to distinguish between physiological exercise-induced cardiac remodelling in athletes, vis-a-vis underlying pathology.
Most recently, the 2017 International Recommendations for ECG Interpretation in Athletes has led to an enhancement in the screening specificity without compromising sensitivity. There is also an attendant improvement in interobserver variability for ECG detectable pathological conditions associated with SCD.10,38
Despite the aforementioned advantages and strengths of employing ECG as a screening tool, the panel acknowledges certain limitations of this modality. First, exercise-induced cardiac remodelling poses significant challenges in the interpretation of the ECG in an athlete. The ECG may still present with false positive results in up to 6.8% of cases even with the international criteria.39 Second, there is a lack of validated criteria for ECG interpretation for Asian people. Third, some conditions associated with SCD may not present with resting ECG changes, e.g. premature coronary artery disease, congenital coronary anomalies, aortic dilatation and valvular heart diseases. Finally, the current evidence on the survival benefit of ECG as a screening tool is mainly from observational studies. To date, only one observational study has reported a reduction in the annual incidence of SCD from an ECG-based pre-participation screening of athletes.40 Evidence from prospective studies on the efficacy of pre-participation screening with ECG remains lacking. In consideration of these potential shortcomings, it is then imperative that the interpretation of the athletes’ ECGs should be deferred to healthcare professionals trained and experienced to do so, such as a sports medicine physician or a cardiologist.
The authors acknowledge that these recommendations could occasionally lead to some athletes being unnecessarily temporally withdrawn from competition but that this is balanced by the benefit of avoiding SCD in young competitive athletes at risk. Furthermore, patients with abnormalities in the initial evaluation who were later assessed by a specialist to be low risk despite the diagnosis of cardiovascular disease, physical activities could be resumed.
The Role of Transthoracic Echocardiography
Transthoracic echocardiography (TTE) plays an integral role in the evaluation of competitive athletes with suspected or confirmed cardiovascular disease. TTE has the capacity to characterise myocardial structure and systolic and diastolic function, valve morphology and function, and proximal coronary anatomy with sufficient accuracy and detail to confirm or exclude the presence of clinically relevant cardiovascular disease in the majority of competitive athletes. The main advantages of TTE include its accessibility, portability, relative low cost and freedom from ionising radiation. In addition, portable community-based TTE in athletes is also feasible with high imaging success rate. Despite all these advantages, at present, the routine use of TTE is not recommended as a first-line investigation pre-participation screening by any professional societies. The impact of this strategy has not been rigorously assessed and the use of TTE outside of carefully controlled settings that are resourced with expertise in sports cardiology is not recommended.41
Participation in Low Cardiovascular Intensity Sports
Statement 4. Routine pre-participation screening for athletes engaging in low-intensity sport (including master athletes) is generally not necessary.
Level of evidence: Low.
Level of agreement: Agree 85%, neutral 15%, disagree 0%.
Evidence-based support for pre-participation screening of athletes participating in low-intensity sports is presently deficient. Several guidelines also do not recommend routine pre-participation screening in low-risk circumstances. For example, the American College of Sports Medicine pre-participation medical screening for non-athletes recommends that for people who participates in regular exercise, medical clearance for even moderate-intensity exercise is not required (even if they have known cardiovascular, metabolic or renal disease, provided they are not symptomatic).42
Existing guidelines also allow the participation in low-intensity competitive sports, even for those with certain cardiomyopathies such as hypertrophic cardiomyopathy, following shared decision making.8,13 The panel agreed that participation in low-intensity sports poses minimal risk and does not recommend routine pre-participation screening in young competitive athletes participating in low-intensity sports in order to optimise healthcare resources while minimising barriers to sports in low-risk situations.
Athletes with Pre-existing Cardiovascular Diseases
Statement 5. Competitive athletes with pre-existing cardiovascular disease should be managed according to established eligibility and disqualification recommendations for:
- cardiomyopathies, myocarditis and pericarditis;
- coronary artery disease;
- arrhythmias;
- channelopathies; and
- coronavirus disease 2019 (COVID-19).
Level of evidence: Low.
Level of agreement: Agree 100%, neutral 0%, disagree 0%.
In situations whereby the young athletes have known or detected cardiovascular conditions that may predispose to adverse outcomes during competitive sports or training, it is recommended that they be managed according to established guidelines, specific to the given conditions, in order to determine their eligibility and disqualification status.
Several international societies, including the European Association of Preventive Cardiology, the European Heart Rhythm Association (EHRA), the European Society of Cardiology, and the AHA/ACC have published updated recommendation statements on the management of athletes with cardiovascular disease, and it is useful to refer to those consensus papers alongside this APSC consensus paper.8,9,11,43
Last, but not least, the COVID-19 pandemic has had a huge impact across the globe and numerous sports participants worldwide have been affected since its emergence. Cardiac involvement, both manifest and latent, can potentially occur even in mild COVID-19 infections, and management of athletes with active or recovered COVID-19 should be guided by emerging and evolving guidelines and advisories to ensure a safe return to sports participation.44,45
Limitations
The main limitation of this consensus document is the dearth of high-quality evidence applicable to the Asia-Pacific region. As the recommendations are developed to provide broad guidance and standardised workflow to healthcare practitioners involved in sports screening, it is important that the approach to each young athlete should be individualised, with due consideration for the type of sports, the level of competition and the training intensities the athlete is engaged in (bearing in mind that training can be more intense than the actual competition8) , the local training and institutional policies in place, and their workforce and logistical resources for pre-participation cardiac screening.
Furthermore, it must be emphasised that these statements are intended for competitive sports and their required training regimen, and not necessarily applicable to recreational sports participation.
Lastly, the clinician should be aware that despite pre-screening, SCD may still occur during competitive sport games and should be prepared for this event (e.g. having automated external defibrillators accessible).
Conclusion
This consensus statement aims to guide medical practitioners in the conduct of pre-participation cardiac screening of young competitive athletes in the Asia-Pacific region, guided by sports intensity. Significantly, the panel proposes pre-participation screening only for athletes involved in moderate- to high-intensity sports and advises that practitioners contextualise the recommendations in accordance with available resources and expertise in their respective country or region. Athletes participating in low-intensity sport are not recommended to undergo routine pre-participation screening, because of the low risk involved and also for healthcare resource optimisation.
The use of sports intensity to guide screening is a unique feature of this APSC consensus paper, and is not a feature in either the 2016 EHRA and European Association for Cardiovascular Prevention and Rehabilitation (EACPR) position paper or the 2015 AHA/ACC scientific statement.1,8 In addition, the APSC consensus included an intensity-based sports classification, which was built upon on the 2015 ACC sports classification framework, and included a substantial number of Asian-centric sports after deliberation and categorised based on intensity.12,30
With regards to the use of ECG, this consensus is similar to the 2015 AHA/ACC scientific statement in that we do not give endorsement to universal ECG screening.8 This consensus stated that ECG is recommended for young athletes participating in high and moderate cardiovascular intensity sports only if certain conditions are met. These recommendations were made after taking into consideration disparities in countries within Asia-Pacific in terms of available resources for screening. This is in contrast to the 2016 EHRA/EACPR position paper’s broad endorsement of ECG as an initial screening investigation for all competitive athletes.1 Lastly, with regards to the utility of routine TTE screening, our APSC consensus is similar to both the American and European guidelines, in that there is currently no evidence to support the routine use of TTE as first line pre-participation screening investigation.1,8